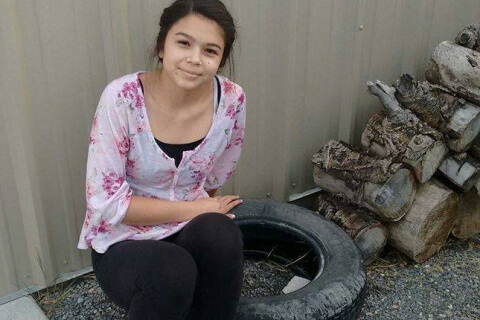
Amy Sampsel’s cry for help for Hailey. Anyone out there listening?
Amy Sampsel shares her medical journal of her daughter, Hailey, in hopes that someone will help her figure out how to take Hailey’s migraines away.

2014
10/17 – Right ankle ligament reconstruction.
Dr A @ Ortho Center. Sat up from surgery and complained of headache in center of forehead, equal on both sides. Always worse with sitting, standing.
10/27-10/28 ER “Migraine Cocktail” & MRI/MRA admitted overnight to Treatment Unit. 11/7-11/15 – Inpatient. Had spinal tap, MRI, MRV, Depakote, IV Prednisone, Some DHE (Nat shortage) Lrg dose caffeine, Thorazine. Left hospital in same pain as arrived minus neck soreness.
11/18- NP at in Neuro diagnosed her with POTS after testing her Orthostatics. Labs drawn, results: BUN high, TSH high, faxed all info to our Pediatrician.
11/21 –Turned 14 yrs old. Started Midodrine 5mg three times a day. Started seeing “sparkles” around this date as she was non weight bearing & on crutches for 6 wks & really just laid down during that time and now moving more.
12/2 – Children’s Hospital Dr B & Dr C. EKG & Orthostatics. Confirmed POTS. Increase Midodrine 10 mg three times a day. Drink 4L of water, 10-12 g salt. Come back to POTS clinic in 3 months. If headache not better in couple wks see Neuro again.
12/8- 1st Appt w/ Dr D and Dx Sudden Onset daily migraines and headaches said common in teens to have with POTS started Amitriptyline 10 mg work up to 5 (50mg total) at HS. Prednisone 10mg (Taper method 4 pills for 4 days 3 then, etc last pill taken 12/19), Gave her 2 injections in occipital nerve of dexamethasone phosphate & bupivacaine hydro (didn’t work). Prescription for Midrin (only took 2 times it didn’t work).
12/29-Appt w/ Dr D started Topamax 25mg a day increase to 100mg. EKG, Experimental treatment numbing medicine inserted through nose. (Didn’t work) Prescription for Imitrex 100mg take with Aleve & Reglan.
2015-
1/5- Tried Nerve block through nose again still didn’t work. Trampoline & Tumbling (did very little) first time went with headache at 6 left with 8/9.
1/8 -Dr D -Nerve block to trigeminal and occipt nerve (6 Injections) using Bupivicaine Hydro, Dexamethasone Phosphate in head migraine at 8 for 3 days and “sparkles” really bad. Relief all but center top band of head. It’s the FIRST RELIEF in forehead in almost 3 months.
1/13-1st Appt w/ Dr E, Internist & Sports Medicine with lots of POTS patients. Started Inderal 60mg, ride exercise bike get HR 125. Referred Pediatric Neurology to rule out never disease.
1/14- Topamax 50mg BID
1/14= Dr F saw nothing of concern. Stay with Dr D or Susan for Migraine help.
1/15- Dr D-Headache at 8-9. Trigeminal nerve block only & shot of 25 mg Phenegren & Stadol. Slept all day. Zero Relief.
1/16-Dr D-IV of 2 Magnesium in each bag, 2L sodium chloride, 5 mg Reglan and 30 mg Toradol. No relief in office. Increased Topamax to 50mg in AM and 75 mg hs.
1/20- Start Adderall XR 10 mg in AM to help Hailey wake up since she is very hard to awaken and doesn’t remember me trying. Also try and help with terrible brain fog.
1/23- Increased Topamax to 50 mg in AM and 100 mg hs.
1/27- Dr D- First treatment of Botox protocol for migraines. Total of 155 units injected. Stop Inderal as Hailey has been crying for several days and saying she wants to die. Not kill herself just not wake up. Amityrptline 50-100mg, Prozac.
1/28- Started Lexapro 10 mg
2/2- Dr D- Nerve blocks brought pain down 3 pts rest of day.
2/3- Visit previous Dr-Labs show Vit D 10.
2/5-1st visit with Dr G-Cardiology/POTS PCMC. Decrease Midodrine to 5mg TID. Started Propanolol 10mg twice a day. Prescription for support hose.
2/5-While riding in car I asked Hailey a question. She could only stare at me and took several minutes before she could answer. She said she could hear me but didn’t really understand what I was saying and had no idea how to talk to me.
2/6- Walked up to chair in school and for a second couldn’t think what to do then remembered oh yeah I need to walk around and sit down. Decided side effect of Topamax and cut back to 75 mg.
2/13-Dr D- IV- Ketorolac tromethamine, Dexamethasone Phosphate, Benadryl, magnesium sulfate, Reglan
2/20-Dr D Nerve Blocks
2/21-Pain Moved from center of forehead to everywhere. “Worse pain ever” IV at PCMC, two bags of fluid, she slept in ER.
2/24- Dr at Eye Exam-said, “eyes look great.” Referred to Neuro Opthamology-Dr H
2/27-PT with Mike- head worse when left
3/2-Dr D- Nerve Blocks. Taper off Topamax can’t see helping may be making brain fog worse.
3/3- PT- head worse and felt “car sick” after
3/5- Acupuncture at- Didn’t help
3/6-IV at Dr D’s- DHE, Magnesium, Reglan, Benadryl, Dexamethasone Phosphate, Ketorolac tromethamine
3/9- Dr D-Nerve Blocks
3/11-Dr (Cardio) POTS stop Midodrine. Consider switching to ? for brain fog instead of Adderall.
3/11-First visit with Psychologist outpatient. Really liked her
3/13-Dr D- Nerve Blocks (only brought relief for 2 hrs) Rapidly start Topamax back to 50mg BID as last 2 wks have been really bad.
3/20- Dr D wouldn’t do nerve blocks as he wanted to wait for Dr Digre visit.
3/24-Saw Dr in headache clinic
3/27-Dr D – Nerve Blocks
3/31- Dr D – Nerve Blocks
4/3- Dr D – Nerve Blocks
4/13- Admitted to Children’s Neuro Trauma Unit and started DHE. She got 9mg before it was called a failure. DHE makes Hailey extremely ill with nausea, stomach cramping and vomiting.
On Day of admittance she was taking:
AM: Modafinil (Provigil) 100 mg Escitalopram (Lexapro) 10 mg
Flurocortisone (Florinef) 0.1 mg Toprimate (Topamax) 50 mg
Vit D3 5,000 Propranolol 10 mg
PM: Midodrine 5 mg Topiramate (Topamax) 50 mg
Amitrypityline 75 mg Melatonin 3 mg one or two as needed for sleep
COQ10 100mg
As Needed taken together no more than twice a wk: Imitrex 50mg repeat in 1-2 hrs as needed, Reglan 5mg and Aleve 220 mg. This brought pain down one point on scale 1-10.
4/18-Moved from Neuro Trauma to Rehab and stopped DHE. While there she did; PT, OT, Acupuncture, Speech, Massage and Relaxation. They also took her off Provigil, Midodrine, Topamax, Propanolol, Amitrypline.
5/7- Discharged from Children’s
5/8-Realized Trazodone was making her feel like spiders crawling on her so stopped it.
5/12- 9/16- PT with Shannon Arnold at Taylorsville location.
5/13- Speech Consult in Taylorsville. The eval came back saying she needs intense speech 3 times a wk for month then weekly have that. Hasn’t happened as insurance refusing to pay
5/14- Dr in Neuro Ophthalmology- eyes look good.
5/15- Dr D- Botox #2
6/9- Stared Northera 100 mg
6/12- Northera 100 mg twice a day
Later went to 100 mg three times a day. Saw no change good or bad. Discontinued it after abt a month.
6/22,6/23- Dr said to try cefaly device per Dr D idea. Hailey didn’t like it.
7/14- Dr D- IV Magnesium, Toradol, 2 bags fluid, samples of Silenor for sleep. Didn’t work.
7/17- Saw Chiropractor said jaw is twisted would not cause headache pain.
8/4- Dr in Provo suggested a Paleo diet
8/7- Dr D- Botox #3, IV-Mag, Toradol, and 2 bags saline. Tried Doxepin didnt work.
8/17-Dr D- IV
8/28- Dr D-IV-Dexamethasone Phoshate, Toradol, 2L fluid, Mag. Helped the body aches and with energy. Lasted rest of day and all next day.
9/18- Dr at adult Neurology Clinic. Blood tests ordered: ANA by IFA, IGG, C-Reactive Protein, CBC w/ Platelets and auto diff, Comprehensive Metabolic Panel, Cortisol Serum Free, Ferritin, N-Methylhistamine 24 hr urine, Rheumatoid arthritis panel w/ reflux, Rheumatoid Factors, IGA/IGG, IGM ELISA, Sedimentation Rate westergren, Serum iron w/total binding cap, Sodium, Urine, Vit B 12 w/reflex to methylmalonic acid, Serum (Vit B12 status), Vit D, 25 Hydroxy
Only thing came back abnormal was ANA elevated to 1.80 and Iron low
9/24- Turned in urine to adult hospital
9/30- Autonomic Lab- Catecholamine Levels and Autonomic Reflex Screen Test (ARS)
10/8-Dr Adult and Automonic Lab at CAMT Neurlogy Clinic- Tilt Table Test and QSWEAT) Her HR went from 55 to 122. Dr Cortez said too much POTS from deconditioning and too much head pain to be just POTS. Go back to Children’s and see Dr Neuro again. Also continue with our POTS Dr’s she’ll stay in loop but doesn’t treat patients until 16.
10/16 Dr D- IV with steriods again. Helped energy and body aches rest of day and all of next.
10/20- Consult at Neuroworxs for PT. Going to have water therapy twice a wk to work on endurance and balance.
10/23- Dr Previous- He diagnosed her with: Trigeminal neuralgia, Chronic daily headache, Other disorders of autonomic nervous system, POTS (postural orthostatic tachycardia syndrome), Symptomatic orthostatic increase in heart rate, Hypermobility syndrome, Dizziness, Other fatigue, Myalgia, Insomnia due to medical condition.
Medication List
Stop Amitriptyline HCl : 50 MG 1 1/2 tablet at bedtime Orally At bedtime
Start CarBAMazepine ER : 100 mg 1 capsule Orally QHS,30 day(s) ,30 ,Refills: 0
Start Diazepam : 2 MG 1 – 2 tablet as needed Orally once a day,30 days ,60 ,Refills:
Continue Lo Loestrin Fe : 1 MG-10 MCG / 10 MCG 1 tablet Orally once a day
Continue Prozac : 40 MG 1 capsule in the morning Orally once a day
Continue Vitamin D-3 : 5000 UNIT Orally
Dr notes: Your POTS appears a type Partial Dysautonomia, related to hypermobility(EDS) , with noted 4x increased in catecholamines. initial tests for mast cell appear to be negative, but should be reconsidered with EDS. As explain, improving POTS depends on how we can improve cardiac output. Stop the amitriptyline as this can worsen the POTS response to catecholamines. 10/24- Dr – IV of
10/26- Dr – Treatment initiated today for her Chronic Daily Headache with noted failure of all treatments to date, refractory.
History of post surgical pain, that is refractory to regular treatment would be consistent with Central hypersensitivie syndrome, with pain amplification at the NMDA receptor site.
40 mg Ketamine, 2 gm Magnesium, and 2 L fluid over 3hrs. Start Clonidine HCl : 0.1 MG 1/2 tablet. No help with pain.
10/27-Treatment Day #2 of 10 today of Chronic Daily Headache with noted failure of all treatments to date, refractory. Ketamine 60mg, 2 gm Magnesium with 2L Fluids. Allodynia on face and shoulders feeling better. No help with head pain.
10/28- Treatment Day #3 of 10. Ketamine 80mg, magnesium and 2L fluids. Allodynia better no help to head.
Brain MRI at King’s no contrast. Results came back normal.
10/29-Treatment Day #4 of 10, Ketamine 100 mg, mag and 2L fluids. Had labs drawn.
Magnesium (GMC, IHC, PAML) – 1.8 Range: 1.8-2.4 – mg/dL
LUPUS ANTICOAGULANT(INHIBITOR) REFLEX on 10/29/2015 Abnormal
PT, Patient (PAML) – 13.8 Range: 13.3-15.8 – sec
TT, Patient (PAML) – 15.3 Range: 15.6-20.0 – sec Flag: L
aPTT, Patient (PAML) – 31 Range: 31-43 – sec
dRVVT (PAML) – 31.5 Range: 31.8-45.7 – sec Flag: L
MTHFR C677T AND A1298C on 10/29/2015 Abnormal
MTHFR Comment (PAML) – SEE BELOW
MTHFR Comment (PAML) – SEE BELOW
MTHFR Result (PAML) – SEE BELOW
Folate (GMC, IHC, PAML) on 10/29/2015 Normal
Folate – 15.6 Range: 3.0-16.0 – ng/mL
Folate (IHC, PAML) – 15.6 Range: 3.0-16.0 – ng/mL
IV made headpain worse.
10/30- Dr. He decided to discontinue IV’s he thinks it’s a failure. Added new diagnoises:
Cervical spine instability, Trigger point of neck, Cervical segment dysfunction Stop Diazepam as her dizziness has increased.
On today’s exam noted that facial pain did increase with cervical rotation to the right, and lateral flexion. Also point tender along C2-C3 spine and paraspinals. Based on failures in the past and noted cervical joint instability secondary to hypermobility, the primary cause of headaches likely cervicogenic migraines, caused by the convergence of the Facial trigeminal V affarent nerves wtih the C1-C4 affarant nerves in the spinal cord, as they decend down first before going back up to the brain on the opposite side of the head.
Recommend MRI of the Cervical Spine, restart Physical therapy with initial goal of mobilization to neutral. A right paracervical muscle nerve block done today due to amount of tenderness, but will likely need a cervical epidural injection. the anesthesiologist will require the MRI prior to the referral.
11/2-PT for Physical Therapy 3x weekly for cervical spine instability and cervicogenic headaches. First treatment didn’t make her worse but also no help.
11/3-11/4 Wore Pulse Ox overnight to check oxygen. Dr called and said every time she falls asleep her oxygen plummets to 62-63. Ordered Oxygen and it arrived, suppose to wear at bedtime.
11/4- Urgent Care- IV-2L of IV fluids with Toradol. Helped with body aches and energy no head relief
11/5- Dr D- Botox series #4 this completes the 1 yr protocol of every 12 wks times four.
11/9- Echocardiogram at Children’s Cardiology
11/10- Cervical MRI done
11/10- Urgent Care- IV-2L of IV fluids were infused over a 3 hour period. She was given ketorolac and ondansetron IV as well. Helped with dizziness.
11/11- Anesthesiologist, At Pain and spine injected her with some numbing med in Right side of neck in I think Cervical 2 he put diagnois: Cervical spondylosis. The injection failed there was no relief from pain.
11/14- Sleep and Pulmonary Specialists- Sleep study. No results yet but when I asked abt waking up with no oxygen tech replied, “Her oxygen was great all night.”
11/17- Echo showed “Extremely poor apical and subcostal acoustic windows-cannot rule out an atrial level shunt.”
For more information on Hailey’s journey, please go to the following link: Hailey Sampsel’s journey