Today is National DNA Day: #15for15 Started April 5th
About National DNA Day
National DNA Day commemorates the successful completion of the Human Genome Project in 2003 and the discovery of DNA’s double helix in 1953. NHGRI began celebrating DNA Day annually on April 25th after the 108th Congress passed concurrent resolutions designating it as DNA Day. The goal of National DNA Day is to offer students, teachers and the public an opportunity to learn about and celebrate the latest advances in genomic research and explore how those advances might impact their lives. 
#15for15 Celebration
Whether you realize it or not, many parts of our daily lives are influenced by genomic information and genomic technologies. Genomics now provides a powerful lens for use in various areas – from medical decisions, to food safety, to ancestry.
April 2018 will mark the 15th anniversary of the completion of the Human Genome Project. To commemorate this milestone and the genomic advances that have been made since 2003, the National Human Genome Research Institute (NHGRI) has launched the ’15 for 15′ Celebration – unveiling 15 ways that genomics has and will continue to transform our world.
We hope that you will join us on this journey and learn how genomics is influencing the world around you. Which genomic advance will you discover today?

DNA Sequencing
Reducing the cost of genome sequencing by a million-fold
April 5, 2018
Did you know… that your genome contains about six billion individual building blocks – and that we can now read the order of all those building blocks in about a day and for about $1000?
Leaps in technology since the Human Genome Project have enabled remarkable genomics-based advances in medicine, agriculture, forensics, and our understanding of evolution.
Our genome (that is, our DNA “blueprint”) – and in fact the genomes of all life forms on earth – are made of four chemical “bases” strung together in varying orders. To study the exact order (or sequence) of someone’s DNA, researchers follow three major steps:
1) purify and copy the DNA;
2) read the sequence; and
3) compare to other sequences.
First they use chemical methods to purify, then “amplify” the DNA in the sample — that means they copy small parts of the sample to reach high enough levels for measuring. The amplification step makes it possible to do DNA testing from very small starting amounts, like those in forensic samples or ancient bones. Then, different methods can be used to determine the order of each base in the DNA sample. Finally, they use computers to compare the sequence of the DNA to a reference sequence (for example, of the human genome), in order to see if there are any differences in the order of the bases.
Technology Advances Since the Human Genome Project
The Human Genome Project opened the door to vast improvements in three major areas:
- the methods used to amplify and sequence DNA, including a million-fold reduction in the cost for sequencing a human genome;
- continually improving the accuracy of the reference “human genome sequences” that everyone can use for comparing newly generated human genome sequences; and
- powerful new computer-based methods for analyzing and comparing many human genome sequences.
As a result, we now have multiple methods for sequencing DNA quickly and inexpensively [see videos in resource section], and we have the computational ability to compare thousands of genomes at once.
DNA Sequencing Has Gone Mobile and Into Space
When the Human Genome Project officially started in 1990, no one knew that it would lead to the generation of over $1 trillion in economic return and the creation of hundreds of thousands of jobs. It brought together scientists from all over the world. In 2016, genomics went beyond this world! Dr. Kathleen “Kate” Rubins became the first person to sequence DNA in space. She used a hand-held instrument to sequence a DNA sample sent from earth, showing that DNA sequencing can be performed in space. In December 2017, fellow astronaut Dr. Peggy Whitson became the first person to sequence microbes brought from earth to the International Space Station itself. Adding this technology to the space station can bring the same advances in medicine and science to space exploration.
Human Genomic Variation
Understanding what makes each of us different and what makes us the same
April 6, 2018
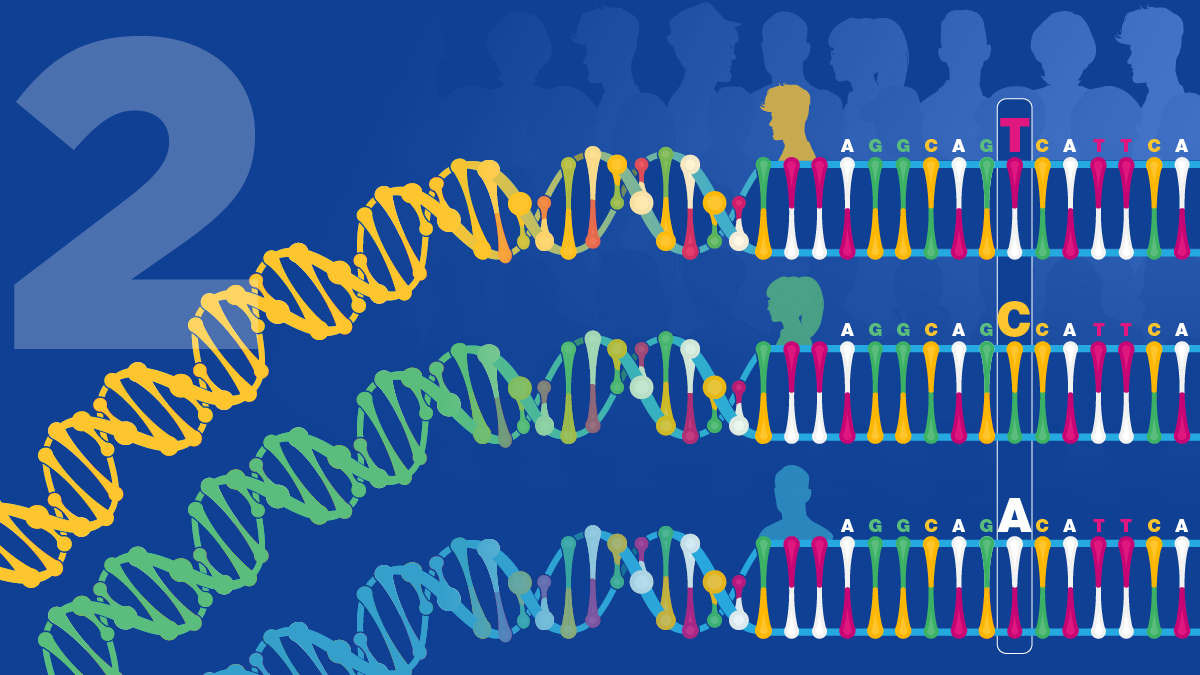
Did you know… that at the base-pair level your genome is 99.9% the same as all of the humans around you – but in that 0.1% difference are many of the things that make you unique?
We have learned that people’s genomes differ from each other in all sorts of ways. Those differences in your DNA help to determine what you look like and what your risk might be for various diseases. But your genome doesn’t entirely define you.
Well before the completion of the Human Genome Project, researchers began developing tools to detect genomic differences between people. When scientists agreed to use the one “reference” human genome sequence generated by the Human Genome Project [see DNA Sequencing], it became easier to determine differences among people’s genomes on a much larger scale. We have since learned that human genomes differ from one other in all sorts of ways: sometimes at a single base, and sometimes in chunks of thousands of bases. Even today, researchers are still discovering new types of variants within human genomes. Human genomic variation is particularly important because a very small set of these variants are linked to differences in various physical traits: height, weight, skin or eye color, type of earwax, and even specific genetic diseases.
The Beauty in Diversity
Rick Guidotti built his career as a fashion photographer until he decided that he wanted to showcase beauty in a different way. Through his not-for-profit organization called Positive Exposure, he began taking beautiful photographs of children and adults with genetic conditions that we don’t always see showcased in magazines or on billboards. Rick’s work has highlighted the beauty in human diversity (much of it caused by genomic variation); you can see true joy in their online gallery, “The New Faces of Genetics And Beyond.” Rick has gone on to create projects like FRAME (Faces Redefining the Art of Medical Education), which is designed to substitute the images of unsmiling children often used in the medical literature and text books with joyous photographs and fun short movies. As Rick says, medical students “are going to be better doctors, because they’ve seen these kids not in crisis. They’ve met these kids not in a clinical environment, but they’ve seen these kids as people.”
The Human Genome Project has also led to a change in our understanding of human traits and how we teach them – one example is eye color. For many years, students were taught that one dominant gene controlled brown or blue eyes and that blue-eyed parents could not have brown-eyed children. Scientists knew that the blue-eyes trait was actually more complicated despite what was taught in schools, but technology developed during and after the Human Genome Project helped pinpoint the actual combination of genomic variants that determine eye color. In fact, at least ten genes each of which comes in several “flavors,” contribute to eye color. It is the combination of these gene variants in a person’s genome that produces the wonderful range of human eye colors. Other traits are even more complicated; for example, around 80% of a person’s height is controlled by more than 700 genomic variants, each one having a very small influence.
Variations in Human Skin Color
Another area where our understanding of biology has greatly advanced is in the genomics of skin color. Unfortunately, for centuries, skin color has been used as the basis for discrimination against some populations, a consequence of the inaccurate concept of human races. We have always known that skin comes in a wide array of hues and tints. Thanks to the work of Dr. Sarah Tishkoff and her colleagues, we now also know that skin color has changed quite a bit over time, with mixing and matching occurring throughout different populations. Sarah and her team visited numerous different communities throughout Africa, working with them to study their genomes. Her work has shown that there are multiple genomic variants contributing to skin color: some make it lighter, some make it darker, and all of them originated in Africa. Throughout evolution, skin color has been affected by the environment. For example, Sarah’s work supports the hypothesis that lighter skin in climates further away from the sun gave an individual a selective advantage (because their skin was able to make more vitamin D and avoid diseases like rickets). In contrast, darker skin color was helpful in climates with more sun (because the pigments in the skin help to prevent sun damage and skin cancer).
This new understanding of the importance of both genomics and the environment has led Sarah and other genetics researchers to call for medical studies to stop using skin color or race as a biological category. Instead, genomic testing for variants that influence traits that are deeper than skin can be used to understand how their genomes might influence their health.
We Are Still Learning
One of the most astonishing things that we have learned about human genomic variation is that we cannot always predict the effect of a given variant. Sometimes there are clear relationships, such as for red hair (the hair color of most redheads is due to one of three single-base changes in a particular gene). But a large study that started in 2012 has shown that each human is walking around with an average of 200 genes that are broken; for about 20 of those genes, both copies (one inherited from each parent) are not working, so there is a “loss-of-function.” Surprisingly, in some people, one of those 20 doubly broken genes was previously thought to be responsible for a genetic disease. We would think a person with such a mutation should be sick, but for some reason they are not! Are they “genetic superheroes?” Or are they just more resilient to these genomic variants for reasons that we don’t yet understand?
Another possibility is that they are “mosaic,” meaning that they have “harmful” genomic variants in some tissues but not others. For example, Joseph Merrick, the subject of the book and movie “The Elephant Man,” is thought to have had a disease called Proteus syndrome, which causes overgrowth of skin or other tissues. In 2011, a group showed that mutations occurred in the gene AKT1 in this syndrome. Each person with the syndrome does not look the same because they have different areas of skin overgrowth, and we now know this is because the genomic variant occurred in a different set of cells. Interestingly, the new abilities to sequence very small amounts of DNA have shown that we are all mosaics, and that the genome in one tissue is not always exactly the same as in another. This is a potential problem for diagnosis; since only the DNA in blood is typically sequenced, mosaic-like variations elsewhere in the body could be missed. Single-cell genome sequencing of neurons in our brains even suggests that one neuron might not be the same as the one right next to it!
Studying genomic variants can also point to surprising new ways for developing medications, such as happened with the gene PCSK9. Many research projects have shown that high blood cholesterol levels raise the risk of developing heart disease. We know that both genetics and environment/diet contribute to your cholesterol level, so scientists have been looking for specific genes that might play a bigger role. By looking at lots of people, researchers found that there are some individuals have unusual levels of cholesterol in their blood. These people have very low levels of “bad” cholesterol and a reduced risk for developing heart disease. Scientists searched through their genomes and found that they carry a rare loss-of-function mutation in a gene called PCSK9. It appears that mutations that inactivate the PCSK9-encoded protein makes people resilient to any type of diet. Scientists immediately realized that if they could “break” this gene in people who have a good copy, they might be able to lower their cholesterol too. They soon designed a drug that inactivated the protein made by PCSK9. This could mimic the protection from bad cholesterol found in the rare people who inherited the mutated PCSK9. Trials of such new medications have now shown they can lower cholesterol and should prevent heart attacks or strokes. We are likely to see more drugs based on naturally occurring loss-of-function variants revealed by genome sequencing.

Cancer Genomics
Transforming how we study, diagnose, and treat cancer
April 9, 2018
Did you know … that we are increasingly able to detect cancers by testing just a blood sample? Or that we are moving toward treating cancers not by where they are found in the body, but by how their genomes have changed?
Cancer is caused by changes in your genome, but advances in DNA sequencing technology are leading to a new understanding of cancer and new ways for diagnosing and treating many types of cancer.
Cancer is a group of genetic diseases that result from changes in the genome of cells in the body, leading them to grow uncontrollably. These changes involve DNA mutations in the genome. Our cells are constantly finding and fixing mutations that occur in our genome as the cells divide over and over again. But on rare occasions, some mutations slip through our cells’ repair machinery, and those mutations can lead to cancer. The Human Genome Project has allowed us to establish what “normal” usually looks like for a human genome, so that we can now tell when changes in our genome have taken place that lead to cancer.
Large projects around the world, like The Cancer Genome Atlas in the United States and the Catalogue of Somatic Mutations (COSMIC) in the United Kingdom, have now determined the genome sequences of thousands of cancer samples of many cancer types. These projects have shown that some cancers have mutations in the same group of genes, even though they may have started in completely different tissues. Many of the mutations activate genes that normally promote cell growth or break genes that normally prevent cell growth. If we know more about the specific mutations that led to someone’s cancer, no matter what tissue it was located in, then we can look for more specific and effective treatments for their cancer.
Lukas’s Story: Using His Genome to Treat His Cancer
Dr. Lukas Wartman, a physician and a researcher at Washington University, has both led cancer genomics efforts and experienced them himself. Lukas was diagnosed with a blood cancer called acute lymphoblastic leukemia (or ALL) in 2003, when he was in his fourth year of medical school. This led him to specialize in treating patients with leukemia, and studying the disease in the laboratory. While his university was helping pioneer cancer genome sequencing, Lukas suffered a relapse of his ALL with severe symptoms. So the laboratory, including Lukas’s mentor, asked if they could study him.
The team compared the genome sequences of his normal cells and those of his cancerous blood cells. In his cancer’s genome, they found mutations in a gene called FLT3. The team then found that there was an existing medication that could be used for treating patients with mutations in this gene. Although it had originally been approved for treating other cancers, not blood cancer, they tried it anyway. Lukas started taking the medicine on a Friday, and his blood counts already showed better results by Monday. After a number of weeks, the leukemia cells were no longer detectable in his blood, meaning his cancer was in remission. He will still need more treatment, but Lukas would not have survived without the results of the genome sequencing that pointed him to a new therapy.
There are over 10,000 clinical trials for new therapies in cancer that are recruiting right now in the United States. In addition, cases like Lukas’ have led to the resurgence of “n-of-1” clinical trials, where doctors can gather enough information from just one patient to try a new therapy. Such trials are aided by patients who share their genomic data with researchers or even openly with other patients. Increasingly there is hope that as clinicians evaluate new cancer patients, they will be able to compare each new case with these large databases that might include positive responses to medications approved for a different cancer but with the same mutation(s), just like Lukas found for ALL.
Blood Tests to Detect Cancer Anywhere
Unfortunately, some cancers are harder to evaluate because looking at their genomes would require difficult and painful biopsies or operations where tiny parts of the cancer tissue are removed for study. This also makes it harder for clinicians to monitor how treatment is working for some cancers because repeated biopsies are just not possible. Recent breakthroughs now allow the detection of circulating tumor DNA (or ctDNA) in the blood of patients instead of directly sampling the tumor. As cancer cells grow very fast and die, they release some of their DNA into the bloodstream. We now have tests that are sensitive enough to detect and sequence these pieces of ctDNA in the bloodstream separately from the normal DNA of the patient – this is called a “liquid biopsy.”
Although liquid biopsies are not yet in widespread use for cancer detection, improvements are being made all the time that move us closer to the routine use of ctDNA tests. One of the current approved uses for ctDNA is to test progression of non-small cell lung cancer by looking for specific mutations in the EGFR gene over time. Liquid biopsies can point to who will likely relapse after treatment, by detecting DNA with EGFR mutations that is circulating in the blood, sometimes better and more quickly than the now-used standard imaging techniques.
When Cancer Runs in Your Family
If you have a number of relatives who have developed cancer, you might be concerned about your own risk. By far, most cancers are not inherited, but there are a few examples of inherited cancers like Lynch syndrome (also known as hereditary non-polyposis colorectal cancer). This disorder is due to inherited mutations in any of six different genes, and leads to an increased risk of different types of cancers, most often in the colon. Breast cancer is another example; again most cases are not inherited, but men or women who have inherited mutations in the BRCA1 or BRCA2 genes have a much higher chance for developing breast cancer than other people. As we learn more about the genomic changes predisposing a person to cancer, we have been able to make screening tests available to many more people. The specific DNA sequences of the BRCA1 and BRCA2 genes were even the subject of a legal case that went all the way to the United States Supreme Court, who ruled that the sequences of your genes could not be patented. Before this ruling, only one company could provide BRCA1 or BRCA2 testing in the United States, but now there are a number of companies who can help if you’d like to have genomic testing for hereditary causes of breast cancer.
Human Origins and Ancestry
Illuminating human and family origins at the genomic level
April 10, 2018

Did you know … that your genome helps uncover the history of your ancestors, both near and distant?
Advances since the Human Genome Project allow us to compare genome sequences among humans, living and long-deceased, and to trace our collective ancestral history.
Where did different humans come from and how are we related? These are among the most common questions that humans ponder. The Human Genome Project produced a reference human genome sequence that scientists now regularly use to compare with newly generated genome sequences. This reveals genomic changes that have occurred in different populations over time, which provides a more powerful way to decipher the various stories of human origins and ancestry.
Ancient DNA Tells Our Species’ History
Nearly 20 years ago, scientists developed techniques for extracting small amounts of DNA from ancient samples, like bones or fur or even soil, and used very sensitive methods for sequencing the extracted DNA [see DNA Sequencing]. Genomic studies like these have allowed us to examine human genomes from around 500,000 years ago when our ancestors (the species Homo sapiens) were diverging from other similar species, such as Homo neanderthalensis or Neanderthals.
So far, we have learned that Neanderthals took a different path than humans in their migrations around the world, but there are still traces of Neanderthal DNA sequences in our genomes today. These small stretches of DNA may influence traits that have helped people survive in some way, making it more likely to then be passed on to their children. For example, a 2017 study found that some Europeans still carry Neanderthal-like sequences that influence their circadian rhythms, making them more likely to be a morning person or a “night owl.” In contrast, some DNA variants might have just happened in one population and not another. The same study found variations in the MC1R gene that lead to red hair were extremely rare or nonexistent in Neanderthals, so that trait seems to be human-specific. As we find better ways to isolate DNA from ancient remains and improve our DNA sequencing technologies, we will learn more about our species’ history.
Human Migrations Out of Africa and Around the World
What happened when humans began to migrate out of Africa and move around the world? Genome sequencing of Africans living in different times – from as long as 6000 years ago to today – has revealed that humans divided into different groups and moved around the world at multiple times. In Southern Africa, local hunter-gatherers and then herders appear to have been replaced by Bantu farmers around 2000 years ago. As humans migrated into Europe, the genomes of different groups also began to retain different variants. One 2008 study looked at about 200,000 specific places in the human genome where people are different from each other [see Human Genomic Variation], among a collection of Europeans. The patterns of genomic variants among different groups could be used to reproduce the map of Europe with 90 percent accuracy. Even more surprising, when a new European person’s genome was analyzed, the researchers could predict where that person was from within a few hundred kilometers. More recent studies in the United States also show that genomic variation coupled with genealogical records can be used to infer birth location quite accurately.
The DNA Discussion Project: Ancestry and Identity
As we learn more about genomic variation in specific populations and groups, more robust tests are being developed to help you decipher your ancestral origins. But, before you take one, you need to be aware that the results of these tests may alter your perception of your family history and even of yourself. The DNA Discussion Project, started by West Chester University professors Drs. Anita Foeman and Bessie Lawton, aims to encourage greater understanding of the science of genomics, the social construct of race, and the perception of ethnicity. For example, as Drs. Sarah Tishkoff and Carlos Bustamante’s research groups showed in 2010, an African American individual in the United States has, on average, about 75-80 percent West African ancestry and about 20-25 percent European ancestry. Students at West Chester shared that while they had always been told that their family had Native American ancestry, the DNA tests revealed this was not the case.
Video produced by 42 Degrees North Media
With such ancestry testing, some people have discovered that their ancestral origin is not what they thought, while others have found that close relatives are not who they thought. Some adopted children have used DNA tests to track down their birth parents, or to find previously unknown siblings. Meanwhile, some studies report that, depending on the country, anywhere between 1 percent and 10 percent of children are raised thinking that someone is their biological father when, in fact, that person is not. Ancestry testing can lead to delicate and complex situations, so it is important to think about the potential consequences before using such tests.
Agriculture
Empowering farmers to improve the food supply
April 11, 2018

Did you know … that in agriculture, genomics enables farmers to accelerate and improve plant and animal breeding practices that have been in use for thousands of years?
The ability to read genome sequences coupled with technologies that introduce new genes or gene changes allows us to speed up the process of selecting desirable traits in plants and animals.
Let’s say that you were a farmer thousands of years ago. If you found a couple of plants that were more productive than others, and you needed more food, you might experiment to see if you could combine (breed) those two plants in some way to get better seeds for a better yield in next year’s harvest. If you were successful and able to plant those seeds, and then in future generations chose even more productive plants to breed together, over time most of the plants in your field would be even more productive. This is called selective breeding. From Mendel’s experiments with peas, we learned that plants have genes that influence their traits such height, seed shape and color. From genome sequencing, we can now find specific variants in those genes that contribute to desirable traits and select for those genomic variants in future crops.
Genome Modification Techniques Allow Selection for Desirable Traits
The ability to read genome sequences coupled with technologies that introduce new genes or gene changes now allow people to speed up the ability to select for desirable traits in plants and animals. By mimicking natural processes, scientists can selectively add traits like resistance to herbicides in plants. The resulting offspring have been called genetically modified organisms (or GMOs). One example is “Golden Rice,” which is a rice strain that has small bits of corn and bacterial DNA added to its genome. These extra genes allow the rice to produce beta carotene (a vitamin A precursor). The lack of vitamin A affects millions in Africa and Asia, causing blindness and immune system deficiencies.
Those who developed Golden Rice see it as a potential tool for fighting vitamin A deficiency and saving lives. In 2015, they were given the “Patents for Humanity” award by the U.S. government. However, as with other GMOs, there are practical hurdles and societal controversies that have prevented its widespread uptake. Golden Rice has not yet reached the yields of conventional rice in many of its field trials, posing a financial barrier for farmers who might want to switch. At the same time, protesters who do not believe that GMOs are safe for humans have vandalized some of the field trials. Many studies have shown that consuming GMO plants does not pose any more risk to humans than eating non-GMO plants, but the controversy continues in many countries.
Genome Sequencing for Better Breeding
Genome sequencing is also now used in cattle farming and with other animals, adding speed and precision to selective breeding methods. In Brazil, scientists are using genomics to characterize specific sequences in hundreds of bulls at a time, allowing them to select for increased meat production and use of pasture feeding (to avoid grain supplementation). They hope that this will lead to animals that grow faster and convert grass to meat in a more sustainable manner over time.
Illumina Inc.
As the human population on earth grows, so too does the need for secure food supplies and delivery to billions of people. World hunger had been on the decline, but it is now on the rise. To meet these demands, farmers will continue to incorporate genomic technologies into their practices, whether through genome monitoring during conventional breeding or genomic modifications with older or newer technologies, like CRISPR/Cas [see Genome Editing]. At the same time, scientists will continue to sequence the genomes of more and more crops, teaching us about differences among them related to their DNA.
Genomics for Food Safety Monitoring
One of the most important agricultural advances in the 20th century has been the ability to move food around the globe to people who need it. Unfortunately, food supplies sometimes have unwanted guests along for the ride, such as bacterial pathogens. When people eat the contaminated food, they can get very sick or even die, so it’s important to find the pathogens and eliminate them. The U.S. Food and Drug Administration (FDA) has an entire network set up for whole genome sequencing of bacterial contaminants in food, called GenomeTrakr. In 2017, this database had over 5800 bacterial sequences added on average each month, as scientists tracked new outbreaks in the quest to keep our food safe. FDA scientists work closely with others from the U.S. Centers for Disease Control and Prevention, the U.S. Department of Agriculture’s Food Safety and Inspection Service, and state health departments to identify bacteria that might cause outbreaks from food contamination. Rounding out this network, the National Center for Biotechnology Information keeps track of what foods are linked to each incident, as well as in human patients who got sick. These information sources have been crucial for lowering the impact of foodborne illnesses over time.
Genomes at Work
Learning how our genomes serve as blueprints for life
April 12, 2018

Did you know … that just knowing the genome sequence of an organism only reveals part of the story – and that it is also important to determine how that organism interprets its genome and uses that information to build and operate itself accordingly?
Less than 2 percent of the human genome corresponds to “genes,” but we know other parts are important for regulating and translating the genome as well as responding to environmental influences. Even still, the job of large parts of the genome remains a bit of a mystery!
When scientists started the Human Genome Project, they didn’t even know how many genes were in the human genome. It then came as a big surprise to learn that human beings only require roughly 20,000 genes! Those 20,000 or so genes are encoded by less than 2 percent of our genome. What is the rest of it doing? And how does each cell read and interpret its genome?
How Your Cells Use Their Genome
Although it’s appealing to think of the genome sequence as the “book of life” for an organism – one that contains all of the biological instructions to develop and operate that organism – we now know that the DNA bases are only the starting point.
It can be useful to think of a genome and how it works by a set of maps. Some maps are very simple; they may represent basic information such as the locations and intersections of roads. Such a simple map would be like the sequence of a genome: it would reflect the structure of the road, but would not give information about how it’s used. As genomic technology improved, more complicated maps could be developed, adding many features and layers of information to a simple genome map. For instance, we learned that the basic sequence of a genome has stop signs and start signs added to it, just like roads do, and that these additions direct the “traffic” of proteins that bind to DNA and allow the cell use the genome. Other technologies also became available to map traffic patterns, revealing the presence of high- versus low-traffic area. In a genome, a high-traffic area might be a place where many genes are turned on by proteins binding to the DNA. These areas call for multiple layers of regulation, just like in a city where you might have high-rise buildings on top of a busy street with a subway underneath. In low-traffic areas, a genome can have deserts of hundreds of thousands of bases with no genes, with little sign of proteins binding the DNA. In the 15 years since the completion of the Human Genome Project, scientists have developed better and better methods for constructing three-dimensional “satellite” maps of genomes, where we can see what proteins bind to what DNA sequences in a single cell and at a specific time. It is the different patterns of “on” and “off” genes that helps produce the different types of cells that makes you, you.
Video produced by 42 Degrees North Media
Some of the stop and start signals that direct our cells to translate the map of our genomes are called “epigenomic modifications.” Epigenomic modifications are often chemical groups that are added or subtracted from DNA bases or proteins that bind to DNA that change the way genes are read. Such modifications can be passed on as cells divide, even though they are not strictly changes in the DNA itself. One of these epigenomic modifications is called methylation. As a human is developing, some early cells start to become brain cells. Specific small chemicals (called methyl groups) are added onto the DNA in front of genes that won’t be needed for brain cells. Here, the methyl groups act like stop signs: in all future brain cells, the methyl groups will make sure the genes that aren’t needed stay turned off. This and other cellular tools in your cells are how the body makes sure its roughly 20,000 genes are used correctly by each cell type. Did you know that your cells were so smart?
Although methyl groups are not changes in the sequence of the DNA bases, epigenomic modifications like these can act like mutations by directing if the bases are read or not.. For example, in cancer cells, methyl groups are often inappropriately added at specific places in the genome. Now the cells grow out of control because the “stop” signs have been added in front of genes that would keep the cell in check. Some cancer therapies are drugs designed to stop these methyl groups from being added where they should not be, like the medicine azacitidine which is used in some blood cancers.
How Epigenomics Affects You
In the last 15 years, we have learned how the environment influences how the genome works through epigenomics. Here’s one example: in the winter of 1944-1945, Germany had blocked the food supply to the Netherlands, and the population suffered a terrible famine. The effects of the “Dutch Hunger Winter” could be seen in the children born from women who were pregnant during the famine. The babies from mothers who were malnourished only in the beginning of their pregnancy, but then had normal levels of food later, had a greater frequency of obesity throughout their lifetimes; they also had higher risks of chronic diseases like diabetes when compared to their siblings who were born before or after the famine. In a striking finding, the children of these babies were also found to have higher risks for the same chronic diseases. So it seemed like something could be passed down through generations, but not changes to the DNA sequence itself. Sure enough, research has shown that the methylation patterns in the DNA were altered in these children, and the altered patterns were inherited by their own children, changing their health outcomes.
We know that diet directly affects methylation because nutrients in our food provide the methyl groups themselves. This means that the diet of either parent can affect their children and grandchildren. But it’s not just diet – there is strong evidence shows that smoking can change methylation patterns as well. Epigenomic patterns can also be altered by drinking alcohol during pregnancy, leading in extreme cases to fetal alcohol syndrome. While not everything is controlled through epigenomics, these modifications to our DNA play a central role in how the genome carries out its work. But they aren’t the only controls we’ve learned about through the Human Genome Project.
What the Rest Of the Genome Does
If only 2 percent of the genome’s bases are used to encode proteins, what is the other 98 percent doing? Some of the genome’s bases help determine its structure. There are areas like the telomeres, the ends of each chromosome, that are very important. Just like the caps on the end of your shoelaces, telomeres keep the ends of your chromosomes from fraying. Some of the other parts of your genome position the genes in the right places to be read by the cell’s machinery. So, although those bases might not encode proteins, the genome cannot function without their presence.
dark matter” or “junk DNA,” we are learning that the 98 percent has all kinds of important roles. Some parts called “ultraconserved elements” have kept the exact same sequence for millions of years in mammals, even though they don’t contain genes. Why would that be? Recent studies suggest that deleting these elements causes brain changes and could lead to some neurological diseases like Alzheimer disease, although we are still learning why.
Here’s another fact that might be a little creepy: up to 45 percent of your genome is actually leftover DNA from viruses that infected mammals over millions of years. We haven’t yet worked out what much of that old viral DNA is doing, but we know it’s contributed to at least one very important mammalian trait: exchanging nutrients between mother and baby through the placenta. The rest of the genome includes regulatory elements, including areas that influence genes to be expressed at the same time in response to the environment; transcribed sequences that the cell reads but does not use for making protein; and material which acts as a hotspot for your chromosomes to exchange information with each other.
Rare Genetic Diseases
Ending diagnostic odysseys for patients with rare diseases
April 13, 2018

Did you know … that there are truly rare people born all the time?
Around 350 million people on earth are living with rare disorders – this is a disorder or condition with fewer than 200,000 people diagnosed. About 80 percent of these rare disorders are genetic in origin, and 95 percent of them do not have even one treatment approved by the FDA
The ability to read the human genome quickly and cheaply has led to substantial advances in discovering the causes of rare disorders. Many families have gone through years of “diagnostic odysseys,” going from one specialist to another trying to find the root cause for their family member’s rare disorder. It is difficult to overstate the relief that genomic testing has brought to many of these patients and families, not just for themselves but eventually for other affected families who are finally able to connect and share their challenges. In the last 10 years, a large number of patient groups have formed after the genomic cause has been identified for a specific rare disorder. These groups allow family members and patients to communicate with each other through social media or conferences. Perhaps more importantly, many of these patient groups are accelerating research on rare diseases by recruiting patients with the same condition to participate in scientific studies. When families band together, their efforts sometimes shrink the path for establishing the genetic basis for a rare condition from decades (and unfortunately many patient lifetimes) to a year or two.
Bertrand’s Story: Families Banding Together
Matt Might and his family provide one such genome sequencing story. Matt and his wife Cristina knew almost right away that their son Bertrand had some difficulties, which became worse over time. They obtained testing for a number of known genetic conditions, but Bertrand did not have any of them. In 2010, they enrolled in a study at Duke University that used DNA sequencing to help children with undiagnosed disorders. It took over a year, but they finally learned that Bertrand had a mutation in each copy of a gene called NGLY1.
Bertrand’s mutations meant that he had no functioning copy of this gene, and therefore no N-glycanase 1 protein (which the gene encodes). His disorder was so rare that mutations in this gene had never been documented, and he was the first known human to lack this protein. So, he helped define the list of symptoms observed when someone does not have the NGLY1 protein, including an inability to produce tears or properly move some muscles. Knowing Bertrand’s symptoms and mutations quickly allowed for the identification of at least 15 other children with the same disease, and the establishment of the NGLY1 Foundation to support research about the disease and pursue possible treatments. In 2015, Matt was one of those invited to the White House by President Obama to celebrate the announcement of the Precision Medicine Initiative.
Sonia’s Story: Looking for a Treatment
Another inspiring story of how genome sequencing can transform the life of someone with a rare disease comes from Sonia Vallabh and Eric Minikel. After a rare disease took her mother’s life, they learned through genetic testing that Sonia had inherited the same mutation that causes familial fatal insomnia, or FFI. This fatal disease, caused by abnormal proteins in the brain called prions, makes the brain start functioning abnormally, with symptoms that eventually include a total inability to fall asleep. Sonia and Eric quit their jobs and careers to go back to graduate school in biomedicine, and are earning their doctoral degrees from Harvard Medical School by studying the mutations in the PRNP gene that cause prion diseases like FFI.
Along with their colleagues, the couple have already conducted a groundbreaking study on the impact of PRNP mutations. We already knew that different PRNP mutations lead to different conditions based on where in the gene the mutation is located. However, Eric and Sonia’s team made the surprising discovery that PRNP mutations are more common than we previously thought, and these mutations don’t seem to cause disease at the same rate in everyone who has them. In other words, there are still factors we don’t understand that determine whether or not a PRNP mutation will lead to certain symptoms. This information opens up more questions, but it also points to important directions for any future studies of this and other rare diseases.
Science For Everyone
If you have a family member who has seen a number of medical professionals but not yet received a diagnosis, they could apply to the NIH’s Undiagnosed Disease Network. This national network of medical and research centers aims to help both individual patients and to contribute to the understanding of how the human body works. That’s what Zarko Stanacev did – after 12 years of mysterious symptoms but no diagnosis, his genome was sequenced and interpreted by a team including Dr. William Gahl at the U.S. National Institutes of Health. They found a mutation in the gene NLRP3, which causes abnormal inflammation throughout the body. After only one treatment with a medicine to dampen this inflammation, Zarko’s symptoms improved.
Just like Sonia and Bertrand, he has contributed to medical research by allowing his genome to be sequenced and studied.
Video produced by 42 Degrees North Media
Additional Resources:
- Science Didn’t Understand My Kids’ Rare Disease Until I Decided to Study It: Sharon Terry, TEDMed 2016
- HudsonAlpha Institute for Biotechnology – The CSER Program: Tiana’s Story
- The PEARLS Project: Positive Exposure Ambassadors’ Real Life Stories
- Rare Action Network State Action Center
- NIH – Genetic and Rare Diseases Information Center
Resources for Educators
- Career Profile: Genetic Nurse, Video
- Career Profile: Physician Assistant, Video
- PBS/WETA – The Gene Doctors Videos
- American Society of Human Genetics – Rare Disease Diagnosis Through Sequencing & Bioinformatics Hands-On Activity
- NIH – Genetics Home Reference
Resources for Healthcare Providers
- NIH – Genetic and Rare Diseases Information Center
- NIH – Undiagnosed Disease Network (UDN)
- American College of Medical Genetics and Genomics: Find Genetic Service Providers
- NLM MedGen – Detailed Information on Human Medical Genetics Conditions
- NLM GeneReviews – Clinically Relevant and Medically Actionable Information for Inherited Conditions: E-Book
Posted: April 13, 2018
Pharmacogenomics
Choosing the right medication at the right dose for each patient
April 16, 2018

Did you know … that the sequence of your genome can determine how you respond to certain medications?
Understanding pharmacogenomics, or tailoring a person’s medications based on their genome, would not be possible without sequencing the genomes of many people and comparing their responses to medicines.
One of the most important uses for DNA sequencing is not to just sequence one human genome – but rather to sequence many human genomes to understand how genomic differences relate to different traits. Some such traits reflect physical characteristics (like eye color), whereas others can be used to help in the clinical care of patients. Scientists in the field of pharmacogenomics study how specific variants in your genome sequence influence your response to medications.
Influencing How Medicines Work
In order for our bodies to use some medicines properly, the cells in our bodies must make a few chemical changes that convert them into an active form, just like we do when we eat food. Then, these active forms of the medicine must get to the right places in the body or inside cells to do the job that we want them to do. If we want to make sure this happens, it makes sense that we would target our bodies’ pathways involved in changing the medicine’s form or in getting medicines to the right places. For example, you probably know someone who takes an antidepressant. Many of these medicines get to the right places by interacting with a protein called ABCB1, which works like a traffic cop on the outside of your cells.
Given ABCB1’s important role in controlling traffic, you might imagine that if someone has a genomic variant that changes the shape or function of their ABCB1 protein, they might have a different response than usual to any number of medicines. We now know that is the case for some antidepressants, as well as other medications like statins for cholesterol and certain chemotherapy medicines. As a result, there are at least 18 pharmacogenomic tests for variants in ABCB1 listed in the NIH’s Genetic Test Registry, with suggestions that you be tested for these variants to help determine the correct dose for certain medications.
Video courtesy of Mayo Clinic
Stopping Dangerous Side Effects
Healthcare professionals and researchers are constantly seeking both to optimize medical treatments and to avoid adverse (or negative) reactions to treatments, which are estimated to affect between 7 percent and 14 percent of hospitalized patients. This makes adverse reactions a large cause of added days spent in a hospital, and the fourth leading cause of death in the United States.
One scary example of such an adverse reaction is Stevens-Johnson syndrome (SJS), a severe allergic reaction also called “scalded skin syndrome.” It can be caused by infections, but also by very common medications like ibuprofen, anti-seizure medicines, or antibiotics. Patients may go from taking two pain pills to ending up in the hospital burn unit fighting for their lives if SJS progresses to a worse condition called toxic epidermal necrolysis (TEN). TEN is diagnosed when patients have shed at least one-third of the skin off of their bodies. Needless to say, anything we can do to prevent this allergic reaction is vitally important.
In Taiwan, married scientists Wen-Hung Chung (a physician) and Shuen-Iu Hung (an immunologist) noticed that SJS/TEN was much more common in patients taking carbamazepine, used to treat epilepsy and seizures, or allopurinol, used to treat gout. They showed that this was due to genomic variants in the HLA-B gene. Not surprisingly, this gene helps control the immune response. As a result of their work, the country of Thailand has implemented genomic testing before these medications are prescribed. The results of this “pharmacogenomic test” are used to decide whether it is safe to give a specific patient certain medicines, like carbamazepine or allopurinol. Thailand’s government even covers the cost of this testing, and the frequency of SJS/TEN has been drastically reduced. We have since learned that different ancestries are associated with different HLA-B genomic variants, so countries may need to take different approaches to monitor which medications are most likely to be linked to SJS/TEN.
Video courtesy of Mayo Clinic
Relationships are Complicated
Understanding pharmacogenomics would not be possible without sequencing the genomes of many people and comparing them, and then comparing their response to medicines. But we have also learned that a person’s genome sequence is not everything when it comes to medication responses. The human body is a very complicated machine, and the instructions written in our DNA are just part of the process.
There are some cases, as with the breast cancer treatment tamoxifen, where a small study showed that there might be a relationship between someone’s response to the medicine and a variant in the CYP2D6 gene. However, this finding did not appear to be true in a larger study that involved many more people. That’s why at this time, the U.S. Food and Drug Administration (FDA) labeling for tamoxifen does not recommend CYP2D6 pharmacogenomic testing, but the issue is still being reviewed as more research is conducted.
Another gene in the same CYP family, called CYP2C19, has variations which affect how your body can use clopidogrel (more commonly known as Plavix). This medication is a “blood thinner” which helps prevent blood clots, and thus reduces your risk of strokes or some heart attacks. If your CYP2C19 protein is not working properly due to a mutation in the gene, then you will not be able to process clopidogrel, and you need either a different dose or a different medication. As it turns out, these variants in CYP2C19 are also more common in those with Asian ancestry. Although testing for variants in this gene is also not routinely recommended, you may wish to speak with your healthcare provider about the test if you are given a prescription for clopidogrel, particularly if you have East Asian family members.
 Noninvasive Prenatal Genetic Testing
Noninvasive Prenatal Genetic Testing
Revolutionizing health assessments before birth
Did you know… that DNA sequencing now allows us to test for specific genomic variants in a fetus using a small sample of a pregnant mother’s blood?
Pregnancy can be a stressful time, and for many years prenatal genetic testing has required invasive procedures with associated risk. New DNA sequencing technologies have now truly revolutionized the field.
Less than a decade ago, women seeking prenatal genetic testing, such as for a condition like Down syndrome, had to undergo invasive procedures to get a fetal DNA sample. These procedures (such as amniocentesis and chorionic villus sampling) also posed a low risk to the pregnancy itself.
The advent of highly sensitive and efficient methods for DNA sequencing has allowed a totally new approach for prenatal genetic testing, at least for the initial screening test for a new pregnancy. Specifically, these new methods allow the detection of the very small amounts of fetal DNA that naturally circulates in the mother’s blood during pregnancy. Pregnant women now have the option of getting a new type of prenatal genetic test, one that doesn’t pose a risk for miscarriage. It involves a simple blood draw from the pregnant women. This is called cell-free fetal DNA testing, or more commonly, non-invasive prenatal testing (NIPT), and it can be performed very early in the pregnancy. The uptake of NIPT around the world has been remarkable, with literally several million pregnant women getting this test each year. However, it is important to know that the American College of Obstetrics and Gynecology strong urges that that other tests should be used beyond the initial NIPT before any decisions about a pregnancy are made.
Talia and Dan’s Story
After their second pregnancy ended in miscarriage, Dan and Talia grew concerned that they might have serious genetic risk factors that would affect future pregnancies. They chose to have NIPT during their third pregnancy, and were relieved that the test performed with Talia’s blood sample did not any chromosomal abnormalities in the growing baby. They went on to have a healthy baby boy. Stories like theirs are becoming more common thanks to advances both in genomic technologies and in improving access to care. Dr. Diana Bianchi, the Director of the NIH’s Eunice Kennedy Shriver National Institute for Child Health and Human Development, said in 2017 that “Just like Google or Airbnb changed how research and booking a room works, noninvasive prenatal genomics is altering the obstetrician profession around the world.
Marin’s Story
Mothers who have noninvasive prenatal genetic testing may not realize that it can also reveal things about their own health – that’s what happened to Marin Mejia, who had NIPT while pregnant with her daughter Owen. She and her doctors discovered from NIPT that Owen did not have any chromosomal abnormalities. But the test also showed that Marin had cancer, which had spread to several organs. The NIPT detected cell-free DNA from Marin’s tumor cells, just like circulating tumor DNA tests developed in recent years [see Cancer Genomics]. Marin’s medical team monitored her condition carefully, and delivered Owen two months early so that Marin could have cancer surgery and begin chemotherapy. In hers and other cases, the availability of NIPT allowed the medical team to prepare for treating both the mother and the baby.
Implications For Our World
Like many new technologies, NIPT is generating significant discussion about its ethical implications. Such prenatal testing is mainly used to detect an abnormal number of chromosomes, such as a trisomy. Down syndrome is a trisomy of chromosome 21, and NIPT for detecting Down syndrome and other chromosomal abnormalities is being widely implemented in some health systems (for example, the National Health Service in the United Kingdom). Since about 50% of Down syndrome children have heart defects, NIPT can be helpful by giving notice to the pediatric team, who may need to plan for surgery soon after birth. Parents can also begin to prepare for raising a child with Down syndrome or any genetic condition detected by prenatal testing.
However, because NIPT can be performed early in pregnancy, some parents might choose to terminate a pregnancy based on the results. This has led some advocates to question whether conditions like Down syndrome might eventually be eliminated from the population or whether parents who choose to have children with trisomies will face future discrimination. The Nuffield Council for Bioethics, based in the United Kingdom, has also raised concerns that NIPT might be used for selective termination solely based on the sex of the baby. With future advances in genomics technologies, it is likely that we will be able to detect other genetic conditions very early as well. With this will come the need to continue thoroughly considering the ethical implications of such new prenatal testing opportunities.
Enhanced Forensics
Establishing more robust methods for DNA-based forensic analyses
April 18, 2018

Did you know … that forensic analyses of DNA were being used well before the completion of the Human Genome Project, but newer approaches are speeding up and greatly improving the process, and larger DNA databases are making searches more powerful and more widely available?
The National DNA Index in the United States now contains information from over 16 million people and has been used to aid in over 387,000 investigations.
Have you ever wondered how those detectives on TV and in the movies actually use DNA analyses to match a person to a crime or to determine the identity of a person by their remains? This is how it works behind the scientific scenes. In the 0.1 percent of the human genome sequence that differs between people [see Human Genomic Variation] are a number of areas where very short stretches of DNA are repeated over and over. These regions arecalled “short tandem repeats” (or STRs). As these stretches of DNA are passed from one generation to the next, they often experience a gain or loss of one of their repeats. At a specific place in the gene TPOX, for example, there are a series of repeats of the four bases GAAT. You might have 10 copies of that GAAT in your genome, while your neighbor might have 14. Since the repeat doesn’t affect whether TPOX works or not, it doesn’t matter to you or your DNA how many repeats are present. But these changes from one generation to the next lead to differences among STRs across the human population. The British scientist Sir Alec Jeffreys realized in 1984 that by determining the repeat numbers at enough of these STRs across the genome, he could generate a “DNA fingerprint” that was almost unique to each individual’s genome.
DNA Analysis For Human Identification
As new, more powerful technologies for amplifying and sequencing tiny amounts of DNA became available [see DNA Sequencing], scientists teamed up with law enforcement officials to improve the use of DNA analyses for crime solving. In the United States, the Federal Bureau of Investigation created the Combined DNA Index System (CODIS) in 1990. Today, a CODIS forensic profile combines information from analyzing 20 different STRs across the human genome. In theory, the combined data generated for this panel is specific enough to identify one person on earth.
In practice, gathering samples and accurately analyzing the DNA can be problematic. We leave our own DNA behind us all the time, through stray hairs, skin cells, or other materials. This means that samples collected from a crime scene might be a mix of multiple people, and could potentially lead to the real perpetrator of a crime to not be identified. Or, in cases of mass casualties or environmental disasters, many samples might be mixed together or subjected to high pressure, moisture, or temperature. Advances in genomic technologies, including DNA sequencing, are allowing for more precise identification, in some cases using DNA samples collected years ago. For instance, forensic scientists are still working to use DNA analyses for identifying remains from the World Trade Center site after September 11, 2001 and soldiers from the Vietnam war.
DNA forensic analyses are only as good as the people performing the tests. In some cases, samples might get mixed up in the laboratory or statistical calculations may lead to erroneous conclusions. Groups like The Innocence Project use DNA analyses to exonerate people accused of crimes by showing years later that their DNA does not match the sample(s) collected years earlier at the scene.
Missing Persons Found Through DNA Analyses
When DNA evidence is being used in missing persons case, the generated DNA profile will often include markers from mitochondrial DNA and the Y chromosome. Children only inherit mitochondrial DNA from their mother, and sons only inherit the Y chromosome from their father. One example of the use of mitochondrial DNA is the work of Dr. Mary-Claire King with the Grandmothers (Abuelas) of the Plaza de Mayo in Argentina. A group of grandmothers whose children and grandchildren were taken and given to other families donated their own DNA to help find their family members. These abuelas have been working for over 30 years; in 2014, one of the founders named Estela de Carlotto was reunited with her own grandson, marking the 114th child found through their efforts.
PBS Newshour
DNA-Based Predictions
As we improve our ability to analyze ancient DNA samples [see Human Origins and Ancestry] and to understand how our genomes encode our traits, we are gaining interesting insights about what humans looked like in the past and now. Recently, genomic analyses of a set of 10,000-year-old human remains in the United Kingdom (called “Cheddar Man” because he was found in the Cheddar Gorge), allowed scientists to predict what some of the first Britons might have looked like. According to the researchers, Cheddar Man and his relatives would have likely had dark skin, dark hair and light eyes. More recently, scientists have been working towards developing a “police sketch” based on analyses of DNA collected at a crime scene. While DNA variation cannot yet predict an exact facial appearance of a person, it can suggest some traits that can be useful for investigating a crime, like hair color and eye color. The limits of this technology have been explored in an art installation where DNA from discarded chewing gum and cigarette butts was analyzed and used to create sculptures of what the person might have looked like. While still highly speculative, forensic scientists may be able to add such an approach to their toolkit along with other lines of evidence for deducing some elements of a suspect’s physical appearance.
Microbes and Microbiomes
Advancing the study of individual and communities of microbes
April 19, 2018

Did you know … that your body contains many more microbes (including bacteria and viruses) than human cells? And, even though some microbes can cause dangerous infections, you can’t live without others?
Viral and bacterial genomes might be small, but they are packed with information and some surprises about evolution and human health.
When you think of bacteria or viruses, what comes to mind? If you’ve been sick recently, you might not have good thoughts about them.
In 2018, infections from the influenza virus have been particularly rough. A big difference between 2018 and 15 years ago when the Human Genome Project was completed, is that genomics is now used routinely to track influenza virus infections, in real time, as the virus spreads across the country. These data are used to help design the vaccine used for our annual “flu shot.” Even so, just one mutation in the virus’s genome can make a big difference in the severity of someone’s infection. Beyond influenza, the most advanced genomics technologies are being used to track infections caused by the Ebola and Zika viruses as they spread and mutate.
TED-Ed
You may have also heard of situations where the overuse of antibiotics in both the medical and agricultural fields has contributed to bacteria becoming resistant to antibiotics, because with more exposure, bacteria that spontaneously develop resistance survive and reproduce more in this new environment, spreading this trait to the next generation. Now that we can track various microbes’ genome sequences very accurately, we can see that antibiotic resistance most often happens when bacteria trade their DNA back and forth transferring the resistance trait. DNA sequencing of many, many bacterial species has now shown us that there has been rampant transfer of genes throughout history from early species of bacteria to those in existence today. These findings should make people think about the overuse of antibiotics in our world, since in the most extreme cases of infection with antibiotic-resistant bacteria can lead to serious illness and even death.
Microbes Make You Who You Are
Besides the microbes that make you ill, there are also “good” microbes. We contain multitudes of microbes (bacteria, yeast, and viruses), called our “microbiome.” We would not be able to properly digest food without them living in our gut, or to have a working immune system without regular exposure to these microbes. However, things can also go wrong with your gut microbiome, such as when infection with the bacterium H. pylori leads to ulcers – this discovery led to the Nobel Prize in 2005. But, for the most part, our gut bacteria are huge helpers; they even train our own immune systems on what is “good” and what is “bad” in the microbial world. In another story related to our microbiome, we acquire millions of microbes from our mother at birth, including ones that live in our throats and quickly spread to keep out other, more harmful species. Genome sequencing has shown us how diverse our microbial communities are, and we will learn even more as the NIH’s Human Microbiome Project finishes its work in 2018.
Video courtesy of Kurzgesagt – In a Nutshell
We Can Engineer New Microbes
Now that we have learned so much about microbial genomics, what else can we do? The field of synthetic biology has emerged directly from advances in DNA sequencing technologies, allowing for the design and construction of new biological systems. Teams from around the world are manipulating microbial genomes for applications in energy production and medicine. There is even the International Genetically Engineered Machine Competition (or iGEM) in which thousands of students compete each year to build new systems using standard parts called BioBricks. In 2016, a winning high school team from Taiwan constructed a new strain of E. coli, a famous bacterium that lives in your gut, that can detect levels of poisonous metals in Chinese medicines.
Direct-to-Consumer Genomic Testing
Accessing information about your genome from your home
April 20, 2018

Did you know … that anyone can buy a test that will read specific places in their DNA and provide them with information about their genome?
Advances in genomics since the Human Genome Project have led to an explosion in at-home, or “direct to consumer” genomic testing. You can even seek genomic information without involving a healthcare provider in ordering the test or delivering the results. What are the pros and cons?
There are now numerous companies offering you a service to learn more about yourself or your family through DNA testing – maybe you’ve seen ads on TV or heard them on the radio. The global “direct-to-consumer” (or DTC) genomic testing market was valued at $117 million in 2017, suggesting millions of people are purchasing these tests. In contrast to clinical genomic testing, such as for cancer [see Cancer Genomics] and prenatal screening [see NIPT] in which a healthcare provider orders the tests and provides the results, DTC genomic tests can be purchased online or even at your local pharmacy.
Things You Can Learn from DTC Genomic Testing
One popular application of such DTC genomic testing is for revealing family ancestry or genealogy [see Human Origins and Ancestry]. For example, the company Ancestry.com started as a place to search historical and family records to gain genealogical clues, and has now expanded to offer genomic tests for people who seek information about their genomic ancestry. As of February 2018, more than seven million customers had purchased the test from this company alone. Popular TV shows, such as “Who Do You Think You Are?”, have featured their test and information.
Another prominent company, 23andMe, was established in 2006 with the goal of offering genomic testing directly to people interested in getting DNA-based health, traits, and ancestry information. Some of the information reported back to customers are surprising factoids, such as whether you have dry or wet earwax due to genomic variants or if you are likely to prefer salty/savory snacks compared to sweets. They also offer their customers the opportunity to provide their genomic information to large research studies [see Social Context], such as recruiting 25,000 people for a study on the genomics of schizophrenia and bipolar disorder. These research studies can provide another avenue to advance genomic science and improve human health on a rapid basis.
Risks and Limitations to DTC Genomic Testing
In the last few years, there have been a number of stories involving people who found new family members or famous relatives through DTC genomic testing. Some people have found out that family members who they previously thought were genetic relatives were actually not biologically related to them, or even that their own identity is not what they thought. It’s best to ask yourself several questions before taking any DTC genomic test: Is the company reputable? Is the science behind the test solid and independently validated? Has the specific test you are interested in been approved by the U.S. Food and Drug Administration (FDA) if it is about your health? How will you handle the information from the test? Will you want to speak to a genetic counselor or a healthcare provider about the test results?
Courtesy of the World Science Foundation
Let’s take one example. Some DTC genomic testing companies claim to provide information about a child’s ability in certain sports. You want to find out if your daughter will be a sprinting champion. There is validated science behind the claim that certain variants in the gene ACTN3 control different types of muscle fibers (called “fast-twitch” or “slow-twitch”), and many successful sprinters have the “fast-twitch” genomic variants. But the prediction power stops there. ACTN3 variants are just one factor among many, many others – genomic, environmental, and social. So, even if your daughter does not have the “fast-twitch” genomic variant, that does not mean she cannot become an accomplished sprinter. Looking for genomic variants in children, such as the one for “fast-twitch” muscle fibers, also raises ethical questions. Since children may not be able to consent to such a test and/or they might be unable to fully understand what such testing might mean for them today or in their future, is it okay for parents to have their children tested? Might you treat your child differently based on the results?
Several professional organizations have published recommendations for DTC genomic testing, including the American Society of Human Genetics and the American College of Medical Genetics and Genomics. The National Institutes of Health offers an explanation of how genomic testing is regulated, which can help you investigate a specific test.
The Natural World
Understanding evolution and protecting our biological ecosystems
April 23, 2018

Did you know … that the new methods for DNA sequencing have been used to read the genomes of tens of thousands of organisms, some alive and some extinct, allowing us to redefine the “tree of life?”
Darwin could never have imagined the full complexity of the tree of life, but genomic technologies have been used to illuminate the natural world in amazing ways. We are all connected to every living thing on earth, from plants to animals to microbes, through our genomes.
Genomics helps us understand the biology of organisms across the world: why are some faster or smarter than others? Why have some gone extinct, while others are resilient to environmental changes? What do their genomes teach us about our own?
Have you ever taken a close look at a platypus? It has a bill instead of a nose and it lays eggs, just like a bird. But it also carries deadly venom like a reptile, and it has fur and nurses its young like a mammal. In fact, when the first body of a platypus was shipped from Australia to a museum in England, the curator thought it was a hoax.
In 2008, scientists determined the genome sequence of the platypus. That study showed that the platypus is truly a unique mix of reptiles and mammals, with genes for venom and milk being retained in the same animal lineage over many years of evolution! Similar genomic studies involving thousands of other life forms have yielded amazing new insights into about every branch on the tree of life.
Nature Video
Recent genomic discoveries have forced us to rethink many long-standing, basic assumptions. For example, we have learned that many seemingly “simpler” species have more genes than humans, including the octopus and the water flea. Other species have much larger genomes than humans, including the loblolly pine (7-times larger than human) and a salamander called the axolotl (10-times larger than human!). We have also had to change the placement of some organisms on the “Tree of Life” – like when we learned that turtles are more closely related to birds than to lizards and snakes, or when DNA sequencing showed how much DNA had been exchanged between different types of bacteria over time [see Microbes and Microbiomes]. We’ve even been able to sequence the genomes of extinct animals using preserved specimens, like a museum sample of a Tasmanian tiger and the pelt from a woolly mammoth. Although sequencing their genomes cannot bring back extinct species, these studies reveal what these animals had in common with modern life forms on earth – and this, in turn, teaches us important things about evolution.
DNA Barcoding Identifies Species and Prevents Fraud
Scientists can now use information about short stretches of DNA that are unique to each species to establish DNA “barcodes.” These barcodes distinguish one species from another. DNA barcoding can be used to make complete catalogs of organisms in a certain ecosystem, like on the island of Mo’orea in French Polynesia. Then researchers can more precisely track how the organisms change over time and in response to environmental changes. DNA barcodes also provide insights about the diets of animals through the DNA in their feces, so we can determine where animals migrate and can help to protect their habitats. In a different application, DNA barcoding has enabled food safety experts to monitor the food supply and prevent fraud. For example, they showed that the large side wings of fish called skates or rays were being cut into circles and improperly sold as scallops in multiple countries. Stopping this illegal activity is critical for skate and ray conservation.
Metagenomics Explores Earth’s Biological Communities
Have you ever wondered what organisms live in the air in the New York subway system or in extreme environments like hot springs, or how bacterial communities respond to environmental disasters like the Deepwater Horizon oil spill? Thanks to advances in DNA sequencing, there is a new and exciting scientific field called “metagenomics,” which involves studying all the DNA in an environmental sample. Following sequencing of mixed samples of DNA, scientists perform computer analyses to catalog all the living things that are present based on matches to known genome sequences. Metagenomics is important because researchers cannot always grow an organism in the laboratory to study its DNA by traditional methods. Now such organisms can be studied while existing in their natural community, like the microbial mats in Yellowstone National Park. From nine environmental samples taken in the Times Square subway station in New York City, researchers identified traces of 114 unique bacteria, in addition to other organisms like plants and humans. Metagenomic studies are allowing us to appreciate the complex interactions of our world as never before.
Genome Editing
Altering a genome with unparalleled efficiency and precision
April 24, 2018

Did you know … that in the 15 years since we finished reading the human genome sequence for the first time, we have developed powerful new technologies for editing a human (or any) genomes?
We may not yet have jet packs or flying cars, but the ability to edit genomes precisely is now real. These new methods offer the ability to change the genome in a way that could be passed on for generations. But should we?
Some might think that, once we have decoded (that is, read out) the genome sequence of an organism, a logical next step would be to “edit” that genome – perhaps to cure a genetic disease or to alter the a trait in a plant or animal. Scientists have used laboratory methods to make changes in an organism’s genome for many years, primarily to study its biology or to introduce commercially advantageous changes. For example, you might have seen “GloFish” – zebrafish that now produce a protein that makes them fluorescent. But in 2012, a new technique called CRISPR was developed and has revolutionized genome editing. The scientists who developed CRISPR recognized that they could borrow tools from the immune system of bacteria and develop “bacterial scissors” for surgically editing any DNA in any organism. CRISPR has made genome editing much simpler, faster, cheaper, and more accurate than previous methods, and the method is now used in laboratories all over the world.
Video courtesy of STAT News
Genome Editing and Human Disease
Already, we have seen some exciting early studies that use CRISPR to edit the human genome in an effort to study and, perhaps eventually, to treat a disease. Sickle cell disease causes severe pain and premature death in millions of people worldwide. Scientists have already used CRISPR to remove the mutation that causes sickle cell disease in a mouse model, and are working toward clinical trials in humans. For the latter, scientists will remove blood stem cells from a patient with sickle cell disease, edit the genome of those cells to remove the sickle cell mutation, and then re-insert the modified cells into the person’s bone marrow. Since there are still no cures for sickle cell disease, such a genome-editing approach could be a major advance. Another CRISPR application now entering clinical trials aims to combat human immunodeficiency virus (or HIV) infection. HIV enters human white blood cells and then alters those cells’ genomes. Then, it makes copies of itself to infect the person’s immune system, making them vulnerable to other infections. CRISPR is now being investigated for use in either cutting out the HIV-derived DNA from the genome as well as engineering a person’s genome so that HIV cannot enter their cells. However, it is important to stress that these techniques are still relatively new and very much still in testing mode.
Technical Limitations of Genome Editing
CRISPR editing is not perfect and can even be inadvertently harmful. Although CRISPR is much more precise than previous genome-editing methods, it is sometimes imprecise and edits the wrong place in a genome. This means that it could randomly introduce mutations at the wrong sites rather than the genomic location being targeted. Many scientists are working to reduce this risk of imprecise editing.
Even when CRISPR precisely modifies a genome as desired, the introduced change does not always lead to the expected outcome. For example, some of the studies using CRISPR to combat HIV immediately found that on its own, the virus developed separate new mutations that allowed it to escape the CRISPR edits. These new mutations allowed the virus to start replicating again.
As scientists working on gene therapy for many years have found, there are also important technical issues to consider, especially when considering the use of CRISPR for treating a human disease. In order to get CRISPR-based genome editing to work at the right place at the right time for effective therapy, there needs to be a delivery system that works for that specific body location. This makes the bone marrow and the eye attractive for CRISPR-based therapies because they are more easily accessible; other tissues are not as easy to target with this CRISPR systems. In addition, scientists need to make sure that the human body does not mount an immune response to either the CRISPR tool itself or the components involved in its delivery.
Ethical Considerations
Beyond the technical issues, there are significant ethical issues surrounding the ability to edit the human and other genomes. Let’s start with ourselves: so far, most CRISPR studies have focused on editing somatic (tissue or body) cells, so that none of the changes would get passed on to future generations. But CRISPR technologies can be used to edit germline cells, too – these make the sperm and eggs that could carry any genome edits to future children and potentially their children. On the one hand, some might think that it is a good idea to remove sickle cell disease mutations in all future generations. On the other hand, this could open the door to editing genomes to alter other traits, passing the changes on to all future generations. Where would we draw the line?
Is it okay to edit a genome to give a child better eyesight or a few inches more in height? Will we begin to create “designer babies” who might have “better” traits than their parents? As the ethicist and scientist Paul Knoepfler says in his 2015 TED talk, “what is better when we’re talking about a human being?” Many groups are considering the important questions that need to be addressed, including the United States National Academies of Sciences, Engineering, and Medicine. Because of these unanswered questions, a current ban on using federal funds for conducting research on human embryos, and the unknown health risks of genome editing, creating “designer babies” is unlikely to happen in the United States anytime soon.
Like many health technologies and medications, genome editing is also likely to be quite expensive as a medical intervention, at least initially. This could worsen health disparities that already exist based on socioeconomic status. As discussed in the Social Context advance, there is also valid concern about informed consent. Can future parents of an unborn child truly give fully informed consent for that child to have their genome edited, particularly at the current time when such therapies are not fully tested or proven to be safe?
Gene Drives: Changing the Genome of a Population or Species
Beyond human genomes ethical questions about editing other organisms’ genomes are arising. Consider the mosquito and its unwelcome passengers: the malaria-causing parasite Plasmodium or viruses such as Zika or dengue. Genome-editing technologies can be used to introduce malaria-battling mutations in the mosquitoes’ genome that blocks the parasite from infecting the mosquitoes in the laboratory. This might sound great, but let’s think more about it. Introducing these genome-edited mosquitoes into the wild will not make much difference, because the malaria-battling mutations cannot spread through an enormous mosquito population by regular breeding alone. Our edited genome with the malaria-battling mutation will only be carried by half of the offspring from each pair of parents. After three generations, only half of the mosquito population will have the edited genomes.
Instead, it is now possible to couple the malaria-battling mutations with additional genomic changes designed to ensure a rapid spread throughout a population. The second new edit causes the malaria-battling mutation to get passed down to all offspring from that pair. So, when our new mosquitoes mate with “wild” mosquitoes, all of their babies will also have edited genomes, driving the malaria-battling mutation to spread more quickly through the population. In some instances, by thethird generation, all of the new mosquitoes could be malaria-free. This is called a “gene drive” and it has quickly become controversial.
For the first time, we can introduce genomic changes by genome editing and sweep them through populations of an entire species. On the one hand, you might feel like it’s unethical not to introduce such changes if we could stop the spread of malaria. On the other hand, many scientists feel that letting such modified organisms out into the wild is too risky until we understand more about the resulting population-wide consequences. What happens if the malaria parasite develops resistance to the malaria-battling mutations, or comes up with a way to infect another organism? Who gets to decide which organisms are altered in such a large way? Again, the United States National Academies and other organizations are intensely studying the issues relating to these genome-editing technologies, and will issue recommendations as the circumstances change.
Social Context
Fostering an appreciation for what our DNA means for our health, our identities and our culture
April 25, 2018

Do you know … what the slogan “it’s in your DNA” is really all about?
Our ever improving ability to read anyone’s genome sequence raises many issues regarding the social context of genomics. Information about our genomes is starting to become part of our everyday life. Genomic information shapes societal messages about DNA in how we think about ourselves and how others view us.
Companies, universities, nonprofits, and many other organizations have used the slogan “it’s in our DNA” to mean that something is part of their core mission or values. Our understanding of our DNA also extends to our understanding of ourselves: what is in your DNA? Is it the chin that looks like your mother’s or the eye color that is just like your grandfather’s? What story does your DNA tell about the hundreds or thousands of ancestors before you? What continents did they migrate through in times long past? How does your DNA contribute to who you are, or how you are treated within your society?
Continued studies of the ethical, legal, and social implications of genomic advances can help to break down barriers and yield a better appreciation of what truly is, and is not, in our DNA – and what that means to us, our families, and communities and society.
Genomics Raises Ethical and Social Questions
The scientists who launched the Human Genome Project recognized immediately that having a complete human genome sequence would raise many ethical and social issues. In 1990, the Ethical, Legal, and Social Implications (ELSI) Research Program was formally established at the National Institutes of Health (NIH) as an integral part of the Human Genome Project. The research supported by this program, ranges from genomics and health disparities to inclusion of diverse populations in genomics research, to whether people should have the right to refuse to know genomic testing results. Over the last 15 years, this research has greatly advanced our understanding and appreciation of the complex societal implications of genomics.
Consent and Privacy in Genomics

Among the major areas of study in ELSI research are questions about consent and privacy. For example, what do you need to know about a research study that will use your DNA before you agree to participate? That’s called “informed consent.” As new areas of genomics have developed in recent years (like learning about microbiomes), researchers have needed to continually update their guidelines, so as to help people understand the relevant risks and benefits before signing up to be a research participant. Such studies are overseen by Institutional Review Boards (or IRBs), and these boards are made up of scientists, ethicists, and members of the community. An IRB must approve any research projects involving humans.
The widespread availability of genomic data has brought changes to privacy considerations as well. When a test is performed on your DNA, either through a research or clinical program, how is the privacy of your genomic data maintained and does that align with how you want those data to be protected? Since you share half of your genome with each of your parents, and half with each of your children, the information is not just about your genome. Should you be able to stop your relatives from revealing genomic information that could be relevant to you as well? And does that answer change based on what the test is for? Let’s say that one of your parents learns from a genetic test that they have Huntington’s disease, which is often diagnosed quite late in life. This gives you a 50-50 chance of carrying the same genetic mutation for this fatal neurological disease. Some people react to such information by wanting to know right away what their future might be, while others do not want to know.
Another privacy issue that has arisen in the genomics era is when are you entitled to receive all of your data back from a DNA-based research study or a clinical test. In the case of genomic tests, this can often be a lot of data! Research studies do not often return data to their participants, whereas patients are more often provided the results of clinical tests. If you have had direct-to-consumer (or DTC) genomic testing, the companies might have let you download your entire dataset. You might want to share such data with other research groups in order to further science or with other healthcare professionals for your medical care. There are also many questions about what the companies might do with the data, and most companies have user agreements which you must agree to, where they specify their plans up front. This may include sharing your data with others, including pharmaceutical companies and law enforcement. As President Obama noted in 2016, there is a difficult balance in making your data available for some purposes while still keeping them private for other reasons.
Discrimination Based on Genomic Information
Concerns also exist about potential discrimination based on information about a person’s DNA. In 2008, President Bush signed into law the Genetic Information Nondiscrimination Act (or GINA for short). This law is now enforced by multiple federal agencies, including the United States Equal Employment Opportunity Commission. You might have seen posters saying, “Equal Employment Opportunity is THE LAW” – those posters point out that GINA now specifically protects job applicants and current employees from discrimination based on their genetic information. GINA also prohibits health insurers from discriminating against anyone based on their genetic information when determining coverage or rates. At this time, GINA does not cover life insurance, disability insurance, or long-term care insurance. As in all potential discrimination areas, even though legal protections are in place under GINA, it is important to be knowledgeable about your rights and to know if and when they might be abused.
Genomics and Race
The broad availability of genomic ancestry testing is influencing the way we think about the concept of race in America (see Human Origins and Ancestry). We now understand that skin color, as one component of how we think of ourselves, is due to a complex interaction of genes and the environment (see Human Genomic Variation). When we can see the genomic patterns of our ancestors in our own DNA, it might not be the same as how we describe ourselves (or how they described themselves). Large studies of African Americans in the United States have shown that their genomes contain an average of 25 percent European DNA sequences; in the same studies, Latino genomes in the United States show a mix of DNA from African, Native American, and European sources. It turns out that two people who call themselves the same race may be quite different at the genomic level. With our emerging understanding of genomics, we can combine genomic information with historical records and social data in order to study the shaping of concepts such as race.
Video produced by 42 Degrees North Media
Other characteristics often associated with race are part of culture but are not written in our DNA. Racial terms change over time, sometimes even multiple times within one person’s life. For example, the categories used by the national census in the United States have also contributed to what we think of as “race,” but they have changed quite substantially over time. The term “Hispanic” was not offered as a way that a person could describe themselves until the 1970 census, but by 2010, people could answer whether they were “of Hispanic, Latino, or Spanish origin.” Genomics is helping us understand the complex and intertwined relationships between a person’s or groups’ ancestry, ethnicity, and racial identity. The National Human Genome Research Institute is also monitoring the use of race and ethnicity in biomedical research, including any influence on health disparities and inclusion/engagement of underrepresented populations in genomics.
Science For Everyone
If you’d like to try your hand at DNA sequencing, you can check out games like Phylo where you try to align different bits of DNA to find the best match. Or maybe you want to make your own DNA sequencer and improve existing technology even more? The first step could be a DIY thermal cycler that amplifies DNA in samples. For an educational activity on DNA sequencing, check out the DNA Learning Center at Cold Spring Harbor Laboratory.
Additional Resources:
- Battelle Technology Partnership Practice – The Impact of Genomics on the U.S. Economy Report
- Icahn School of Medicine – Whole Genome Sequencing & You Video
- YouTube Playlist – Videos Explaining Different DNA Sequencing Methods
- NHGRI – A Brief Guide to Genomics Fact Sheet
Resources for Educators:
- Career Profile: Laboratory Research Assistant or Technician, Video
- Learn.Genetics – Build a DNA Molecule Interactive
- TED-Ed – How to Sequence the Human Genome Video
- ASM Science Journal – Build the Read: A Hands-On Activity for Introducing Microbiology Students to Next-Generation DNA Sequencing and Bioinformatics
- NHGRI – The Cost of Sequencing a Human Genome Article
Resources for Healthcare Providers:
- Genetics Home Reference – What are whole exome and whole genome sequencing? Website
- American College of Medical Genetics and Genomics – Genomics in Clinical Practice Educational Series Webinars
- The Jackson Laboratory – Clinical Education Resources on Genetics and Genomics Courses
Get Activity Ideas
Celebrate with NHGRI
#UndiagnosedDay has partnered with National DNA Day to raise awareness for the undiagnosed rare disease community!
RUN will be having an event on April 27th! More to come!
- Twitter: @DNAday & @genome_gov
- Facebook: DNADay
Hashtags: #DNADay18 and #15for15
Press Contact
Kiara Palmer
(301) 402-0911
kiara.palmer@nih.gov