RENO
It’s late afternoon and 23-year-old Grayson McClure is lying in the bed that has become his life, talking in his slow cadence about his years enduring a mysterious disease that medical science cannot solve, one many doctors have walked away from even trying to diagnose.
And then it hits, suddenly and painfully, the lightning bolt of symptoms that rule his waking hours and invade his sleep.
His body clenches like a fist. His knees rise to his chest, toes curling fitfully, hips fishtailing, head thrashing; his entire being struck with demonic force. His right arm jerks uncontrollably, reaching back around his head with such violence that his shoulder pops out of its socket.
Inside the darkened bedroom, Grayson’s mother, Kay, is there by his side, as she always is. She scrambles for the syringe already loaded with the prescribed dose of a powerful pain medication she knows will give him momentary peace at best. She injects the drug into the portal embedded in his chest, talking softly, reassuring him. She’s careful not to touch his skin, which might exacerbate his pain. Then she quickly pops his shoulder back into place — her face a thin mask of helplessness.
As the spasms subside Kay returns to her around-the-clock bedside vigil, waiting for the next unexplained attack that can come at any time.
“It happens all day, every day,” Kay, 58, says in a lilting Southern accent. “It happens constantly.”
If a mother and son descended together into hell, this is what it would be like.
Grayson’s unending pain means he has not left his apartment, not felt the sun, in two long years. His skin is pale; his muscles flaccid, diminished by the unending months in bed. The lights are always kept low, the temperature a shivering 55 degrees to help Grayson cope with what he calls “brain fires” that often erupt just as he reaches the normally narcotic precipice of sleep.
For his mother, the daily trial means keeping a baby monitor in each room so she can hear Grayson’s every outcry. She too rarely leaves home. Her son’s physical demands often leave her the desperate choice between showering and making yet another call to another doctor. Her sleep is scattered, an hour or so at a time, often leaving her in an exhausted stupor. Even when she does sleep, she often dreams of needing to help Grayson.
Kay’s burden is one of both frustration and abandonment: not knowing how to help her son while feeling that modern medicine has turned its back on her.
For 11 years, Grayson’s body has been wracked by a series of morphing, unexplained symptoms that have baffled some doctors and sent others into retreat. Several years ago the mother and son left their home in Memphis, Tennessee, to travel the country in search of a diagnosis, presenting Grayson at medical facilities coast to coast. They’ve been in Reno since 2011.
Sometimes, they hold out a ray of hope for an admission that never materializes. One even scolded Kay, telling her to stop treating her son as though he were sick.
Each day, Kay’s routine is the same: She sleeps a few hours after dawn, when Grayson finally collapses. But she’s soon awakened by his cries. That’s when she begins yet another tortured loop: administering medicine, tending to her son, fighting exhaustion, trying to keep her sanity.
“We live in the dark, not in the real world,” she says. “We’ve done it for so long that the real world, well, that just doesn’t matter to us anymore.”
But Kay isn’t giving up. She believes there’s a way, somehow, to determine — and perhaps cure — what bedevils her son. She knows there is a major medical center, somewhere, with the empathy and expertise to help him.
Doctors who have treated Grayson say they have never seen anything like his condition. They blame his gap in treatment on what they call the perverse politics of medicine. Likecriminal prosecutors, many hospitals play a game of statistics, reluctant to take on costly cases they presume they cannot solve. Many see a patient such as Grayson, who requires 24-hour nursing care, as too great a risk.
“Grayson certainly does not fit any mold and, unfortunately that scares a lot of people,” said Bruce Fong, a Reno internal and integrative medicine specialist who has treated Grayson for four years. “His disease is so unique and so traumatic it has sent hospitals running. They simply do not want to put the effort into this case.”
National Institutes of Health officials acknowledge that some patients such as Grayson have been turned away.
“The Undiagnosed Diseases Network is not able to see all who apply,” said Rachel Ramoni, executive director and principal investigator of the UDN Coordinating Center, Harvard Medical Center. “Many of our applicants have come to us as part of a long diagnostic odyssey in search of answers. With that in mind, we have to make difficult, often agonizing, decisions about whom to accept.”
Recently, Grayson’s days have grown even darker. For years, mother and son have rented a Reno apartment to remain close to the two doctors assisting in their case. They cannot return home to Tennessee, not even to visit. Meanwhile, relatives have died, others have been born. Life goes on without them, as their days play out as a two-actor tragedy, staged in a tiny apartment bedroom, with the hum of the air conditioner as a constant soundtrack.
In Memphis, Kay’s husband, Terry, works long hours as an engineer to pay their mounting bills for rent and medicine. Their insurance covers a nurse’s weekly visit, but doctors and other help from home aides are paid out-of-pocket.
Grayson’s condition, which mimics symptoms of other diseases, is worsening. The sudden fits come more frequently, often triggered by walking or other movement. Any facility that takes her son must immediately accept him as an in-care patient, without any preliminary visits, Kay says, because he must be sedated for the expensive medical ambulance-jet flight. Once he leaves the apartment, she knows, there is no return. “We’re trapped here in Reno,” Kay says. “Our doctors here have gotten us as far as they can.”
When not crying out in agony, Grayson suffers in silence.
During his fits he must concentrate to take his next breath, he says. Asked to rate his pain on a scale from one to 10, he insists it’s not possible.
“It burns,” he says of his brain. “That’s all I can say. I don’t know how else to describe it. And nothing has helped it.”
The strain of contantly depending on others sometimes shows. An intelligent man who quotes Plato, likes politics and science fiction, and who once dreamed of becoming an FBI criminal psychologist, Grayson sometimes snaps at his mother for hovering, even finishing his sentences, diminishing his manhood.
He’ll scoff, and Kay will back off.
“I’m sorry,” she’ll say. “I’m sorry.”
But there are moments of tenderness. In the early morning hours, when Kay is most exhausted, she sometimes breaks down emotionally.
There, in the darkness, the son soothes the mother.
“Chill out, Mom,” he’ll say. “Just try and relax.”
“I tell her to stay calm, that everything will be all right,” Grayson says. “I have to keep her sane. I’m not the one reaching out to all the doctors who will not call her back.” He reserves his ire for the physicians who disrespect his mother.
“Like that doctor who sat there and told her, ‘Stop telling your child that he’s sick,’” Grayson says. “I take massive offense at that, the mere suggestion that my parents are to blame for this.”
YEARS OF AGONY
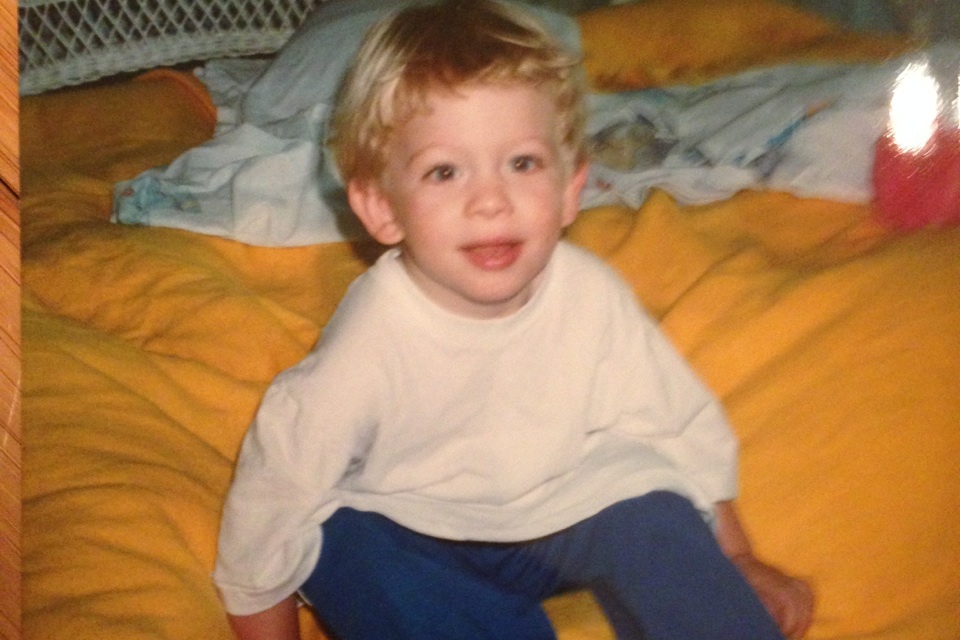
Grayson’s symptoms first appeared in 2005, just two weeks before his 12th birthday.
He was a physically fit sixth-grader with an 11th-grade reading level, the youngest of the couple’s three children. He was running the court in a regular Thursday night church basketball practice in Memphis when his face suddenly became flushed.
He called out to his father, the team’s coach.
“My brain is on fire,” he said. “I don’t feel good.”
He improved a few days later, but the burning returned each time he exercised. He had trouble concentrating and suffered memory losses and panic attacks, unable to write or remember what he was reading. He soon left school. Kay, then a teacher, quit her job to concentrate on her son.
Thus began a decadelong parade to various doctors: neurologists, endocrinologists and researchers specializing in chronic fatigue, metabolic issues, neuromuscular and nervous disorders. None had any answers.
The family visited the Mayo Clinic in Rochester, Minnesota, and research centers inMaryland, Texas and at Tennessee’s Vanderbilt University. Some doctors surmised that the boy suffered from migraines; others doubted whether he was sick at all.
One cardiologist snapped at Grayson: “I see you’re not in school. Even my most serious cancer patients are in school. What’s wrong with you?”
Eventually, Grayson was diagnosed with Lyme disease, but the medication for that and other ailments sent him into uncontrollable convulsions. Each time he tried to sleep, his body would erupt. Soon, Kay surrounded him with pillows so his head wouldn’t slam the headboard.
“His brain would not let him rest,” Kay says. “If he did manage to sleep, his body would soon convulse him out of it.”
She approached major research centers, hoping experts from different disciplines could share information, comparing various pieces of Grayson’s medical puzzle.
When she heard of Fong she moved to Reno. Grayson was treated at an in-house clinic for three months but then became too sick to leave his apartment. Soon, a Northern Nevada endocrinologist took an interest in the case.
Fong remains baffled by Grayson’s condition.
“There just is no category for his disease — and nothing seems to be helping him,” he said. “I’m here to make sure he has enough medication that he doesn’t shake himself apart.”
Meanwhile, Fong is helping find a research center that will accept Grayson.
“It’s a waiting game,” he says. “I’d say we are treading in unknown territory here.”
Dr. Robert Fredericks, an endocrinologist who has invested hundreds of hours in Grayson’s case, says the disease was triggered during puberty. Tests at Baylor University have determined that Grayson suffers from a dozen significant genetic mutations. He believes an experimental drug not approved by the Food and Drug Administration for use on humans could help.
But time is running out, Fredericks says.
“We have run the limit on what we can do safely and ethically from his apartment.”
For Kay, another resource has been Gina Szajnuk, who co-founded a nonprofit group that deals with rare or undiagnosed diseases and who estimates that as many as 30 million Americans suffer from diseases that have yet to be diagnosed.
To help solve the problem, she says, the medical profession must replicate methods of law enforcement and create a nationwide database in which patient records can be traded, diagnosed and subjected to group-think, not dealt with individually.
She knows Kay’s role as the exhausted mother of a critically ill son has become her identity.
“Sometimes, we’ll talk all night, until 4 a.m.,” Szajnuk says. “She’s lonely, apart from family. But she wants to be there for her son. Often, she speaks to me from a darkened closet, where she goes because she doesn’t want to wake him.”
THE WAITING GAME
Surrounded by video games and movies, a slight wisp of a beard growing under his chin, Grayson is lying in bed in a T-shirt and pajama bottoms, explaining why his trained service dog, Yojimbo, is so protective.
The labradoodle’s name means bodyguard in Japanese. Awhile back, when Grayson was at a clinic with others suffering unexplained seizures, nurses and curious passers-by would look into the room, sending the dog into barking fits.
“He knew he was supposed to do something for me, but he wasn’t quite sure what,” Grayson says, his words slowly uttered, his voice a croak. “So this is it.”
Then, another brain storm. Grayson’s body convulses. He cries out as though fighting off a nightmare. Yojimbo — who is trained to respond to seizure patients — jumps onto the bed, looking up with helpless, mournful eyes. Kay struggles to give the injection, but Grayson’s thrashing head has blocked the portal, and she must drop to her knees for the right angle.
Slowly, after 15 minutes, Grayson relaxes, his leg lightly resting on the dog. Sometimes, a single seizure can last an hour or more.
“Oh, buddy, that was a bad one,” Kay says.
Her son sighs.
“Yeah.”
Then he returns to what he calls a “white sleep,” a state of paralysis in which he remains conscious but lacks the energy to move a muscle.
Inside the apartment, the rented furnishings are signs of two lives put on hold. In the living room hangs a deflated Darth Vader balloon as a decoration. At the foot of Grayson’s bed is a placard that reads “To: The King,” awarded by fellow patients because he had the most severe seizures. Next to it hangs a painting of Grayson by an artist there. In the image, he’s sleeping. His eyes are heavy, peaceful. He likes it a lot.
Grayson sometimes is frustrated with his mother’s insistence on jumping too far into the future.
“She always says we’ve got to go someplace else, see the next doctor. I can’t handle that,” he says. “I’m doing the best I can to survive. And it really stresses me out.”
He wants to get better; someday. He longs to scuba dive and return to the martial arts regimen his illness cut short. Sometimes, though, he can’t remember what it’s like to be well.
“It’s like asking a fish, ‘Do you miss breathing air?’” he says.
For now, Grayson simply chooses not to die, knowing his family is there for him; not just his parents but his brother, Jacob, and sister, Lauren.
“This is nearly half my life now,” he says. “I’m playing the waiting game.”
But Kay is anxious. She’s stopped posting Facebook updates on Grayson’s condition for family and friends. She couldn’t bear looking at the happy lies posted by others.
Sometimes, she dreams of moving to another country, where her son can get the help he needs. Her greatest fear is that something will happen to her, leaving him alone.
The other day, she sent an email blast to every Stanford University Medical Center doctor she could find on the Internet. One baffled response said the hospital wasn’t used to people cold-calling for help. A Stanford neurologist reached out to Fong, but no admission decision for Grayson has been made.
And so Kay waits.
She sits in the living room, staring at the muted TV screen as though in a trance; exhausted, not knowing what time or even day it is.
“I’m alone, so very alone,” she says to no one. “But I’m not unhappy.”
In a short while, Grayson will suffer another seizure. He will cry out in pain. And his mother will rush to his side — tired and feeling helpless.
But there.