Rachel Nielsen’s Children’s Hospital of Wisconsin Journey

Recently, my parents and I had the opportunity to go to the Children’s Hospital of Wisconsin to see 2 specialists to hopefully get more answers and treatments for me. I say this like we got the opportunity to go to Disneyland because at this point, for us, it was just as good if not better! In the beginning, I actually really did not want to go at all. It was just another hospital with more doctors to tell me my problems were all in my head and I did not want to hear that again. Luckily, my mom was stubborn and made us go; I will forever be thankful for that!
This trip did not start off on a very good note. When we left Salt Lake City, I fainted on takeoff. We had to switch planes in Minneapolis and I fainted on takeoff again. When we landed in Wisconsin, my body felt 2 times as heavy due to the elevation change. I couldn’t even lift the strap of my feed bag up over my head. I was baffled by this change and couldn’t believe that my mom didn’t feel it.
By the end of the week, we saw 7 not 2 specialists: a geneticist, a motility doctor, a GI, an immunologist, a urologist, a cardiologist, and a neurologist/autonomic specialist. It was so many new faces and so much information thrown at us at once. So to start, we saw the geneticist first. Right off the bat, the geneticist mentioned that he wanted a muscle biopsy from me because he strongly feels that I have a mitochondrial disease. Everyone has mitochondria; they are in every single one of your cells. They are essentially the powerhouse of your cells. They provide the energy your cells need to do whatever that cell needs to do. When mitochondria malfunction, cells die causing systems to shut down all over the body. It affects both genders, it can occur at any age, it is not curable, and it claims more lives than childhood cancer and AIDS combined. It is a brutal disease. From my minute of research on the internet, I’ve found that some people can have mitochondrial disease and have it not affect them at all and then others will ultimately die from it. So in a way, not the best news we could’ve gotten but in another way, we’re so happy to finally be on the path to answers and treatment. I have not been officially diagnosed with mito but we are looking into it.
The geneticist also mentioned a genetic condition known as HHT or Hereditary Hemorrhagic Telangiectasia. This condition is a disorder that causes multiple abnormalities in blood vessels. I’m not completely aware of everything that this would mean, but basically it can cause severe bleeding anywhere in the body. We are looking into this because I am anemic, I have nose bleeds which take a long time to get stopped, migraines, and other signs of the condition. The last disorder we’re looking into is called Ehler’s Danlos Syndrome (EDS) which is a connective tissue disorder, meaning that the stuff that’s supposed to hold your body together isn’t doing a very good job. This could explain why my stomach doesn’t contract anymore and why my bladder has also failed, but this disorder is less likely than the other two.
The next thing I did was a tilt table test and autonomic testing where they observed what my autonomic system does in different situations. This showed that I have a dangerously low heart rate at times and that my vagus nerve is not functioning correctly. The vagus nerve is in charge of sending signals to your digestive tract and regulating certain parts of your autonomic system. For example, sometimes when someone is very stressed, this can mess with the vagus nerve causing it to spasm or be overstimulated, making the person faint. My vagus nerve is damaged which could be part of the reason why I have Gastroparesis and faint.

On Tuesday I did another Gastric Emptying Study (GES) where I ate radioactive eggs, a piece of toast, and had a drink of apple juice. I then laid under a scanner for 90 minutes as it tracked the meal going through my system (or at least, it was supposed to go through). This test showed that my stomach is not working properly at all and after about an hour and 45 minutes, I threw up. The study was supposed to last 4 hours but had to be stopped once I vomited because the technicians could not calculate how much of the meal had actually emptied out of my stomach and how much I had thrown up. On average, people will empty their stomachs in 2 hours. Mine had only emptied around 22% at this time. In a previous GES, it showed that food just sat in my stomach for 45 minutes and then had only emptied 6% at the 60 minute mark.
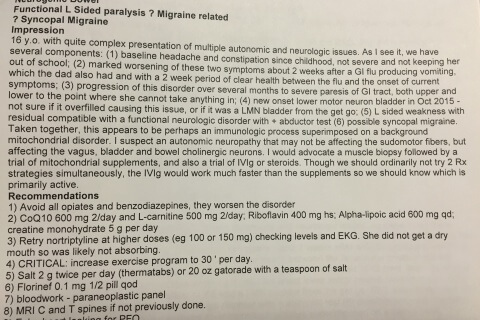
After my study, we saw the Chelimskys. These two doctors are phenomenal and incredibly friendly and nice. They were so welcoming and made the whole stay much less daunting. Mrs. Chelimsky (the wife) is the GI and Mr. Chelimsky (the husband) is the autonomic specialist/neurologist. This is their combined write up after our visit with them. They looked at my history and my current problems and came to these conclusions: They think that I have an immunologic problem superimposed on an already existing mitochondrial disorder that was set off after I got sick in July of 2014. The theory is that this made my mitochondrial disease much worse, leading to severe GI tract paresis. The difference between paresis and paralysis is that paralysis means that everything is completely paralyzed; paresis means that everything is severely hindered or partial paralysis, so things do work just not even close to how they should. They also think I have an autonomic neuropathy affecting my vagus, bladder, and bowel neurons, meaning that when my brain tries to send signals to those nerves, they are getting warped and lost upon arrival, prohibiting certain organ functions.

Wednesday I saw the motility doctor, the cardiologist, and immunology. The motility doctor suggested a lot of drugs to hopefully help with my GI tract paresis and set up my small bowel and colonic manometry tests (motility tests) to see how bad the paresis is. The cardiologist chatted with us and decided to do an EKG, which came back normal and an ECHO which is an ultrasound of the heart that also came back normal. The ECHO was to make sure my heart was structurally sound and the EKG was to make sure my heart didn’t have an abnormal rhythm. He then told me that I needed to wear a heart monitor for 30 days so we can monitor my heart rate when I faint or experience symptoms that lead to fainting. In a normal person, the heart will usually speed up when the person stands up so that gravity won’t pull blood down and out of the brain. The cardiologist is thinking that sometimes my heart does not speed up, making blood pool in my legs and leave my brain, causing me to faint. This would also be due to my autonomic neuropathy. We then saw the immunologist who decided to run blood tests to see if my immune system is in fact attacking me.


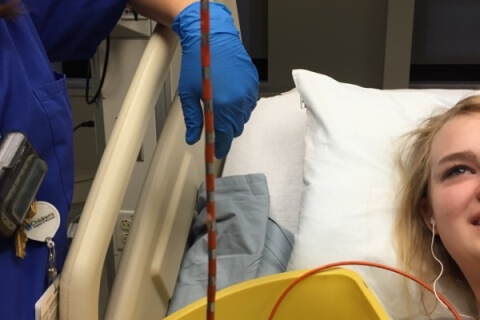

Thursday I woke up at 6:00 am to go into the OR. In the OR, they placed a breathing tube for the duration of the procedure and took biopsies of my esophagus. They then replaced my NJ with a huge catheter that had 30 or so sensors on it to track the movements of the muscles in various places in my stomach and my small intestines. I also had a similar catheter inserted in the other end to track the movements of the muscles in my colon (by the end of the 6+ hour study, my butt was numb from the pain of this thing:P). I woke up and started the study around 11:00 am. First, you do a two hour fasting period where they just monitor your whole system to see what it’s doing. My stomach had a couple of decent contractions, my small bowel was pretty quiet, and my colon did nothing. They then gave me a medicine through an IV to try and stimulate the muscles in my small bowel. This part of the study showed that the muscles in my small intestines are in fact working albeit a little slow.
After an hour had passed since the medication, they had me drink a 400 calorie milkshake to see what my system would do with the food. My stomach barely contracted at all, it was almost a flat line. You could see that it was trying to do something, but it just couldn’t. After an hour had passed since the milkshake, a medication was given to me through the bottom catheter to try and stimulate my colon. This is where the study got really interesting. Usually, you wait another hour after giving the stimulant and you should see one or two good contractions move through the colon. When my hour was up, we hadn’t seen anything and I was having really severe pain, much like my pain when all of this crap started happening back in 2014. The motility doctor was worried about my hydration since it was 5:00pm and radiology wouldn’t be able to replace my NJ until the next morning, so she ordered a liter of fluids to run for another hour and told my nurse to prolong the study until they were done. Still, no movement occurred.
The nurse pulled the nose catheter about 30 minutes before ending my colonic study and pulling the bottom catheter. I literally started a timer and counted down from 60 seconds because I was so excited to get that thing out of my butt!! I can not tell you how uncomfortable that thing was. I know that this is probably more than you ever wanted to know about a colonic manometry but can I just tell you, having a twenty+ foot tube shoved up your bottom and having it sit there for 6+ hours is every bit as awful and probably even more so than it sounds! So when that thing came out you can bet I was super stoked!! So the results of the manometry were: severe paresis of the stomach, slight paresis of the small bowel, and severe paralysis of the colon.
Friday, we saw urology and packed up and went home! They said the only thing they could do for me at this point is place a surgical stimulator into my back next to the nerves of my bladder and hope that improves the function. CHOW has done 20 in the last 2 and a half years with a 60% success rate. Of the 40% that didn’t get “cured” by having it placed, 10-15% saw improvement. So while, the statistics are in my favor, it is surgery and so we’re not going to just jump on it and say, “have at it!” So the plan from here is to get a muscle biopsy to test for mitochondrial disease and then start me on a bunch of mitochondrial supplements that should hopefully make up for what my mitochondria aren’t doing. We’re also talking about starting IVIg therapy. This therapy would be to suppress my immune system to hopefully slow or even stop the progress of my symptoms. At first it would be a week in the hospital where they would hit me really hard with it and then I would get it every month and do it for about 2 days. We’re also considering starting me on steroids to hopefully get my inflammatory markers and histamine levels down which are both crazy high. There is also talk about doing a gastric pacemaker which would be a pacer placed in my abdomen with electrodes hooked up to my stomach. The catch with this is that it doesn’t actually improve my stomach’s condition, it only helps with symptoms. Plus, we can’t just place stimulators and wires all over my body and just hope that it helps.


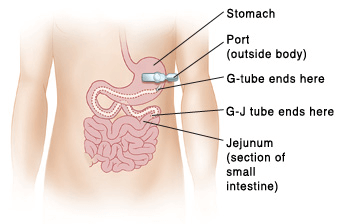
At this point, there is no way to reverse what has happened or cure me, but there are options to get me better. I am getting a surgical G/J tube placed, which will essentially take the NJ out of my nose and put it in my abdomen. The G port will go directly into my stomach so that I can drink things to experience flavor again and then have it drain right out or just drain to prevent nausea, and the J port will go into my small intestines for my formula and meds. This will hopefully drastically improve my quality of life and set us on the right track towards healing. We are also looking into an appendicostomy. This would connect my appendix from my belly button to the top of my colon and then a tube would be placed over my belly button where I would put a medication through to flush out my system. This tube would essentially be doing the work for my colon. My theory is that when all of this started in 2014, my pain was from my colon shutting down and my hope is once we find a way to get this part of me working again, my pain will finally go away (or at least lessen).
Don’t get me wrong, Primary Children’s is a great hospital. They have an excellent staff and help so many people. I love their music therapy, their Sunday church meetings, and most of the nurses are the bomb dot com! But their specialties are with cases that are straightforward such as cancer, heart disease, cystic fibrosis, down syndrome, etc. They could not put me in any of those boxes and so they gave up on me and told me it was all in my head. The best part about going to CHOW was when my cardiologist told me, “We are definitely dealing with something real here.” I’m so ready to finally be heard and to start getting better!
FOR MORE ON Rachel Nielsen’s Journey