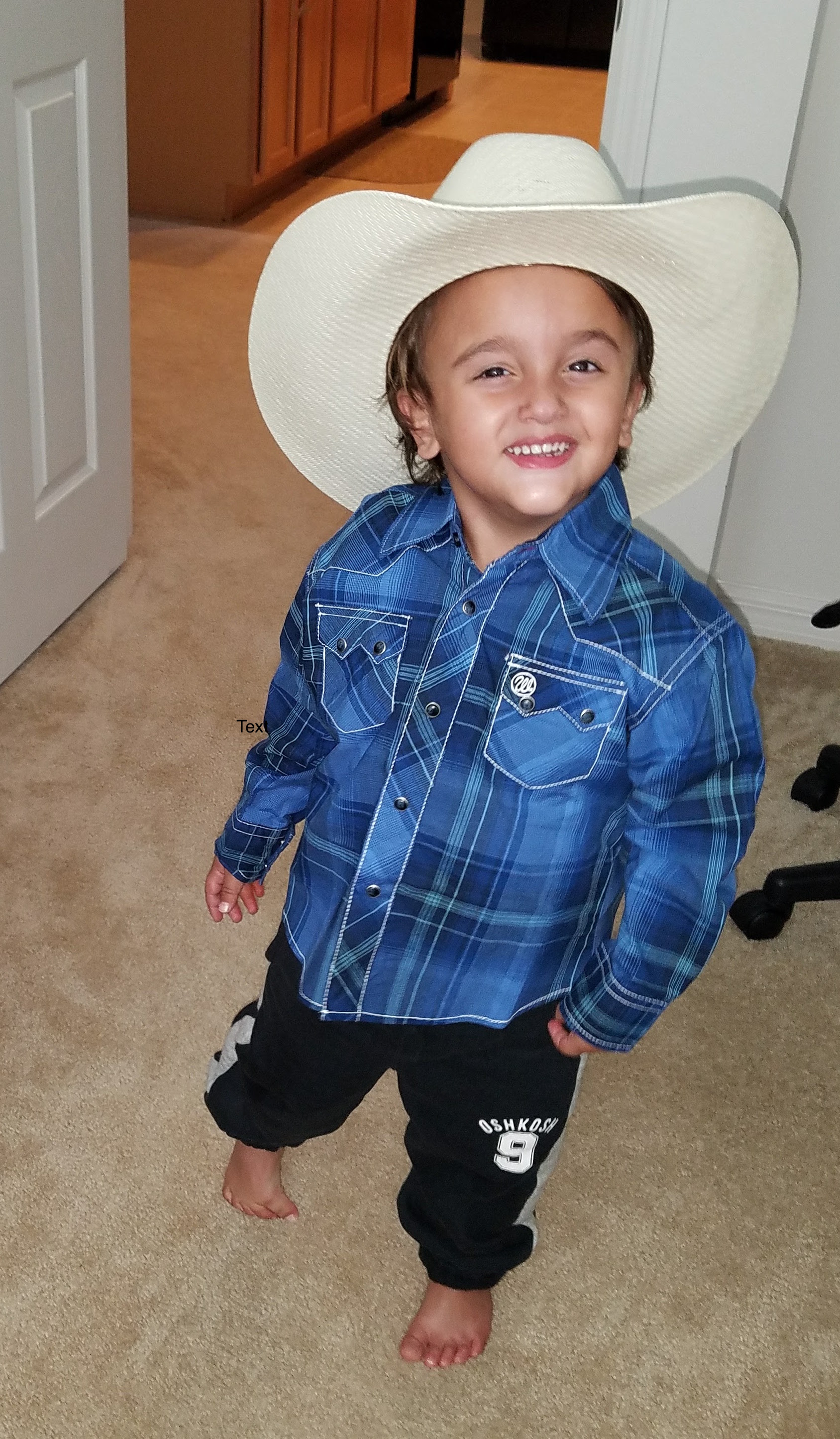
The Rarest of the Rare: Our Miracle Boy by Stefanie B.
 Mothers should always be given credit for knowing their children. Find practitioners who will listen to you and care more about what you know than what they know. I started this blog to help other families find the right path toward health and healing even when there is no diagnosis.
Mothers should always be given credit for knowing their children. Find practitioners who will listen to you and care more about what you know than what they know. I started this blog to help other families find the right path toward health and healing even when there is no diagnosis.
After losing four babies to miscarriages, we thought our daughter would be our one and only. We were surprised and also scared when we found out I was pregnant again. This time, I was 35 years old and our daughter was 6. I was closely monitored and all seemed well until around 27 weeks. Our son stopped growing in the womb and had to be taken out via C-section at 33 weeks. Other than being born anemic and weighing 2 lb. 11 oz, he seemed quite healthy. Two weeks into his NICU stay, he started vomiting regularly and his liver enzymes became mildly elevated.

We took him home after 7 weeks, but within two weeks, we were back at the hospital. His skin and eyes were the color of a mango. His liver enzymes were way off. He was also anemic again and needed another transfusion. They had never seen alkaline phosphatase in the 3000s before. The doctors at our local Children’s Hospital wanted to rule out biliary atresia.
I had serious doubts about this diagnosis.
I reiterated “he gets hypoglycemic” to which they would reply “that’s because he’s tiny”. He was more than tiny…his labs and appearance showed our sweet boy was malnourished.
For a moment, we thought that maybe we should go with their advice and do a HIDA scan. However, after one dose of phenobarbital, his eyes, feet and hands swelled up (doctors said they had never seen anyone have a reaction to phenobarbital, but at this point, the word “rare” meant very little to us).
We left for a children’s hospital four hours away hoping to see one of only two hepatologists in the entire state. His labs were not good, but the hepatologist felt it was developmental and put him on ursodiol, lactulose, vitamin K and Polyvisol. He had blood drawn daily since birth and needed a fourth blood transfusion. The hospital four hours from our home gave him cold blood during the transfusion, and his body temp dropped to 95 degrees Fahrenheit. His glucose was 36. This was one of several times that he nearly died.
On his new vitamin cocktail, his labs improved, but the hypoglycemic symptoms and daily vomiting persisted. He still slept horribly, and I continued to get up with him every hour. I would hold him all night most nights, and if I put him in the crib, I would sleep nearby to check on him constantly. I would often find him in a cold sweat. My gut told me he was having a blood sugar issue, and I would wake him up to give him a bottle of pumped milk or a squirt of glucose in his cheek. Sometimes, after he ate, it felt like he was waking from a coma. His lethargy would immediately turn to energy. He was always hungry, then in pain, then vomiting. At seven months, we switched from pumped breast milk to formula and introduced solids. The vomiting continued. He would scream in pain in the car, and I knew it was more than just reflux. We kept switching formulas.

By eleven months old, his liver was quite enlarged and he looked like he had a pot belly. His ultrasound showed “lesions” that looked like “nothing we’ve ever seen”. Local doctors kept saying “liver biopsy” and “exploratory surgery”. They wanted him to fast for 12 hours! We kept saying “he cannot go 4 hours without food”. My husband and I refused to let anyone put him under.
We traveled to “specialists” within our state and all of them scratched their heads. Nothing explained his unique array of symptoms.
Finally, it was my Welsh-born physician who, upon hearing the long story at my annual check-up, asked me if anyone had mentioned Glycogen Storage Disease. Our boy was eighteen months old by now, and we were tired of having no answers.

I immediately went to my familiar NIH searches and began reading about GSD. I also read information about hereditary fructose intolerance which was similar to GSD but also explained his elevated bilirubin. He had labs that were not explained by either disease, but these diseases seemed to present most similarly to his symptoms.
The nagging question was how did he get exposed to fructose when he was just a few weeks old ? Most babies don’t get exposed until they’re put on table foods . That’s when I remembered the nurses gave him “sweeties” in the NICU every time they would draw his blood. It was the method they used to calm the babies. I kept hoping maybe the syrup was glucose, but when I called the NICU, they confirmed that it was pure sucrose (a disaccharide made of glucose and fructose). That explained his early exposure and liver damage! I was convinced my little guy had HFI. But, GSD made some sense, too.
To cover both bases, we put him on a diet free of sucrose, fructose and lactose (the latter is not tolerated in the most common GSD). This diet is difficult, to say the least. Sugars are everywhere. It took me a month of being told the wrong information by dietitians who knew nothing about HFI to finally get all the sugars out of his diet. We put him on a fructose-free amino acid formula that cost $1000/month, and I prepared all his food to guarantee they were fructose-free. The change in him was miraculous. He immediately stopped vomiting. He went from having no teeth at thirteen months old to getting two or three teeth at a time, his poop became normal and severe diaper rash became a thing of the past. His hair grew. He began sleeping for more than two hours at a time. His hypoglycemia went away. He was no longer yellow. But, he still ate like a bird and was nowhere near being on the growth charts.
 We wanted a definite answer. Without an answer, how could we know the progression of his condition? So, we went out of state to a clinic for rare diseases at one of the top children’s hospitals in the nation. They, too, said they had never seen anything like this. They all agreed something was not right, but they had no idea what it could be. They recommended genetic testing, and if nothing was found, they suggested a biopsy. They wanted to start with a few specific tests and would eventually get to bigger (i.e. more expensive) tests. I wanted to test for HFI immediately, but they said that was not their first test.
We wanted a definite answer. Without an answer, how could we know the progression of his condition? So, we went out of state to a clinic for rare diseases at one of the top children’s hospitals in the nation. They, too, said they had never seen anything like this. They all agreed something was not right, but they had no idea what it could be. They recommended genetic testing, and if nothing was found, they suggested a biopsy. They wanted to start with a few specific tests and would eventually get to bigger (i.e. more expensive) tests. I wanted to test for HFI immediately, but they said that was not their first test.
When we came home, we found a local pediatric medical geneticist willing to test for HFI. The test came back normal! Within a few months, we had many more genetic tests done. The GSD test was normal, too. In fact, all of his genetic testing (tens of thousands of dollars worth) which tested for every known genetic disease came back normal. There were no other tests out there! This was the extent of what was currently available in the world of third generation genetic sequencing.

We were baffled. It was clear that the switch to fructose/sucrose- free was helping. He was taking the amino acid formula and holding it down. We ensured that all his foods were “safe”, but he would eat a few bites and refuse to eat more. After eighteen months of vomiting, food was not his friend. He was sleeping 5-6 hours at night for the first time ever. He was not in constant pain. We HAD to be on the right track.
Our local geneticist, Dr. P, has discovered 40+ genetic diseases in his decades of practice, and he explained that we can only test for what we know right now. He has no doubt that our son has something rare- so rare that it is possible no one else has ever had it or no one else has ever survived long enough to make it known.
Our little man clearly has something that resembles HFI. Dr. P has diagnosed him with “a defect in carbohydrate metabolism at the mitochondrial level with carnitine deficiency”. Our brilliant doc felt there was more to his story and healing, so he put him on a high dose of carnitine (which helps stimulate ATP at the mitochondrial level, improving cellular energy conversion), and our son finally got on the charts for weight and height!
Our treatment is working, as evidenced not just by his symptoms but with improved labs and ultrasound imaging. He has labs so frequently that we are able to see dips and changes in his complicated chemistries that indicate his body is trying to heal but has relapses at times. He no longer has a potbelly, he is no longer jaundice, and he is beginning to accept “safe” foods more each day. I have kept a daily log of what he eats, how he feels afterward, etc. since the day he was born. As he gets older, he will be able to tell us more and a lot of the guessing will go away. We cannot give him live vaccines because the risk outweighs the benefit with mitochondrial conditions and most contain sugars. He eats the same ten foods all the time. I make him “protein muffins”, and he happily eats it while friends gobble down cupcakes at birthday parties.
Having a treatment that is working in the absence of a firm diagnosis tells us we are on the right path toward keeping him healthy and helping his liver heal. We know that this is a journey. It can be a scary path, and we don’t know exactly what his future holds. We don’t know what will happen if he has an infection one day. We don’t know when he can safely go to school. His diet is so restricted, and we live in a world where candy is thrown at children as a reward for answering math problems correctly. Fructose and sucrose are not just in the obvious foods such as fruits and candy. They are everywhere, including medications. We bring his specially made foods and medicines with us wherever we go, and he has a medical ID bracelet in case of an emergency.
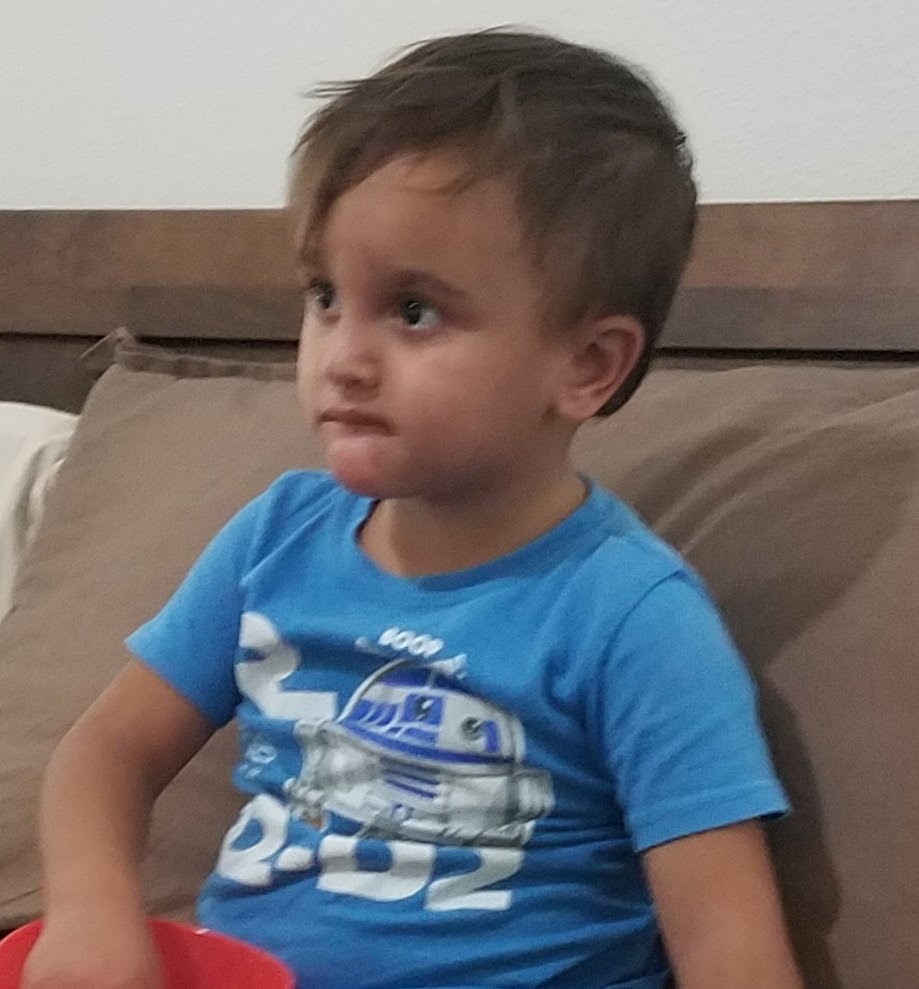 We still don’t know what his exact diagnosis is, but, what we do know is that he is strong, brave, happy, smart and full of energy. We know he is loved beyond measure and that he has the people he needs around him to keep him healthy.
We still don’t know what his exact diagnosis is, but, what we do know is that he is strong, brave, happy, smart and full of energy. We know he is loved beyond measure and that he has the people he needs around him to keep him healthy.
 As Dr. P said, “Even though he will not outgrow this, we will continue to figure out how to manage it – together.”
As Dr. P said, “Even though he will not outgrow this, we will continue to figure out how to manage it – together.”
di·ag·no·sis ˌdīəɡˈnōsəs/ noun 1. the identification of the nature of an illness or other problem by examination of the symptoms. synonyms: identification, detection, recognition, determination, discovery, opinion, judgment, verdict, conclusion “the results confirmed his diagnosis”
For More Information on Stefanie B., please check out rarestoftherare.wordpress.com
Please Contact Stefanie B.
I would love to hear from you. If you are on the same uncertain path, you are not alone.
-Stefanie