Photo by Season Atwater, Aware of Angels
Photo by Season Atwater, Aware of Angels
 UNDIAGNOSED IS A DIAGNOSIS: Living in a Diagnostic Odyssey x 4
UNDIAGNOSED IS A DIAGNOSIS: Living in a Diagnostic Odyssey x 4
By Gina Szajnuk
(This blog was started in February, 2015)
I have three children that are officially diagnosed as undiagnosed. They have an undiagnosed genetic dysfunction.
I am undiagnosed as well. We live in the world of the unknown.
We live in a diagnostic odyssey, times four.

I was born in Madison, Wisconsin and attended the University of Wisconsin – Madison. I graduated with a Bachelor in Communication Arts. I spent my twenties working in the entertainment world for Wes Craven, Jerry Bruckheimer and Miramax Films. I moved back to the Midwest and worked in the NFL and NBA sports agency business where I met my husband, Justin Zanik. He is currently the Assistant GM of the NBA Utah Jazz.
From Chicago, Justin and I moved to the East Coast where I worked in Manhattan for a private equity firm. We waited a few years to have children so that we were financially secure enough that I would not have to go back to work once we had our first child. I was making close to six figures back in 2006. I commuted two hours each way and worked up to a week before my due date.
We had money in the bank and big dreams ahead of having four children and the house with the white picket fence.
By the time we entered our third year of our diagnostic odyssey, our medical bills were astronomical and we could not pay our monthly bills.
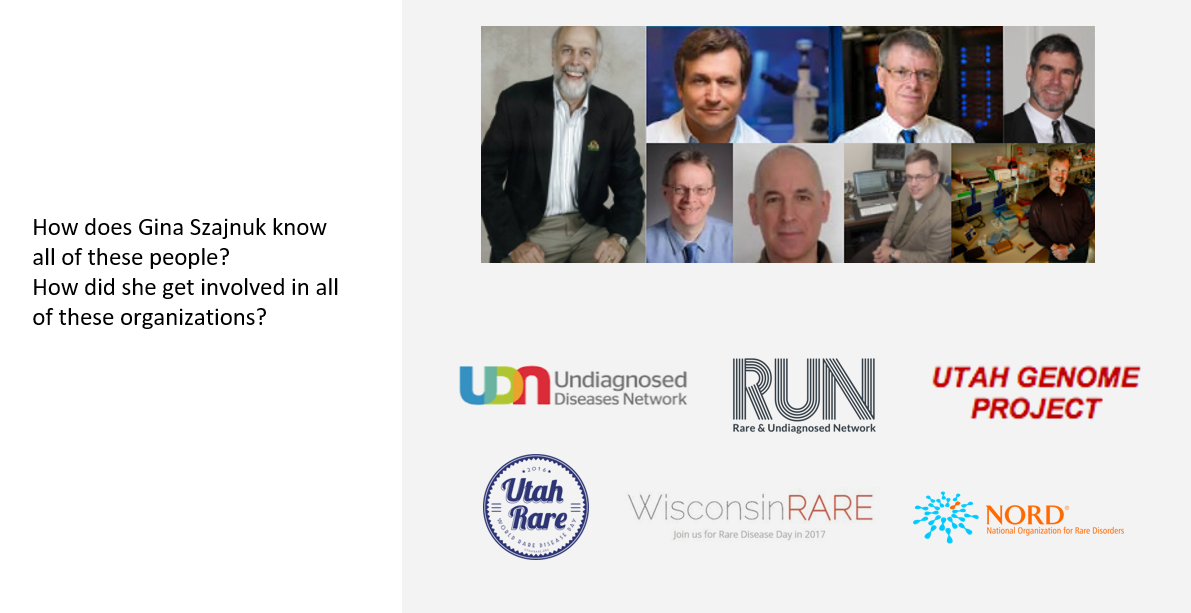 Turning forty-five years old and fighting for the rights of Rare and Undiagnosed families was not something I saw in my future back in those early days of motherhood. I never would have imagined that I would know the names of geneticists like Dr. John Carey, Dr. Howard Jacob, Dr Stephen Kingsmore, Dr. Gunter Scharer, Dr. Lorenzo Botto and Dr. Mark Hoffman. I didn’t see myself working directly with Dr. Lynn and Debbie Jorde and the Utah Genome Project as well as the Undiagnosed Diseases Network.
Turning forty-five years old and fighting for the rights of Rare and Undiagnosed families was not something I saw in my future back in those early days of motherhood. I never would have imagined that I would know the names of geneticists like Dr. John Carey, Dr. Howard Jacob, Dr Stephen Kingsmore, Dr. Gunter Scharer, Dr. Lorenzo Botto and Dr. Mark Hoffman. I didn’t see myself working directly with Dr. Lynn and Debbie Jorde and the Utah Genome Project as well as the Undiagnosed Diseases Network.
I never would have imagined partnering with Dr. Reid Robison, Tute Genomics , to start a nonprofit, the Rare and Undiagnosed Network (RUN), or Chairing Utah Rare in 2016, a coalition of rare disease stakeholders formed to organize Utah’s recognition of Rare Disease Day®. And, I never would have though of becoming the Undiagnosed Advocacy Ambassador for the National Organization for Rare Disorders (NORD) as well as starting #UndiagnosedDay on April 29th, 2016.
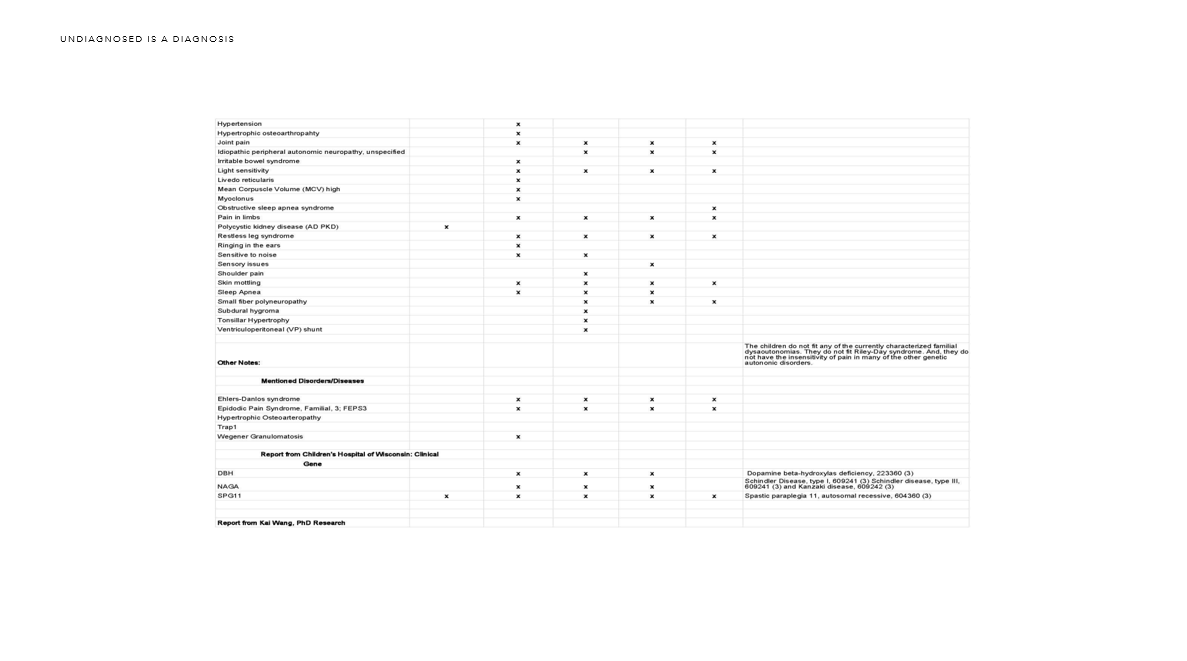
Little did I know when I started having children that I would eventually become educated on whole exome sequencing and whole genome sequencing and dive headfirst into the world of genetics?
Our diagnostic odyssey has come out of the four walls of the many hospitals and into the world of genetics.
 How many people have ever heard or said, “I don’t care if it’s a boy or a girl as long as they are healthy.”
How many people have ever heard or said, “I don’t care if it’s a boy or a girl as long as they are healthy.”
We all want a healthy child with ten fingers and ten toes. Well, what happens if your child is born NOT healthy? Will the answers to the puzzle be found before the child dies? Maybe through newborn screening?
Where do you go if your doctors do not know what the “root” cause is? Do you spend years going to different specialists at multiple hospitals? Do you drain your savings to pay for trips to and from different hospitals in different states? Do you quit your job to stay home to care for your child?
We have met so many amazing people on our journey to find answers. There are so many heartbreaking stories of families suffering emotionally and financially trying to navigate their way through a diagnostic odyssey. All the families have one thing in common. They want answers to help save their children. They want answers to help doctors understand their children. They want answers so they can give their children a better life. We all want our children to live their lives without pain and suffering. We all just want our children to live.
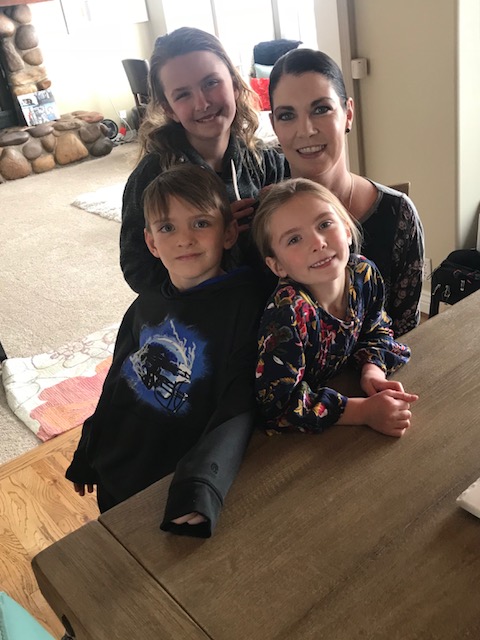
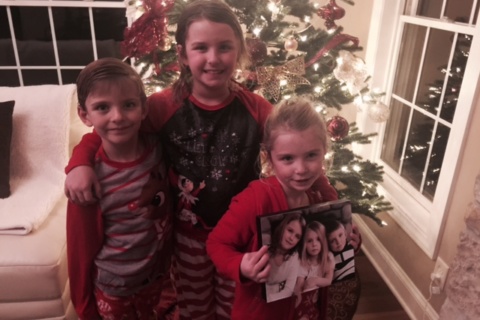
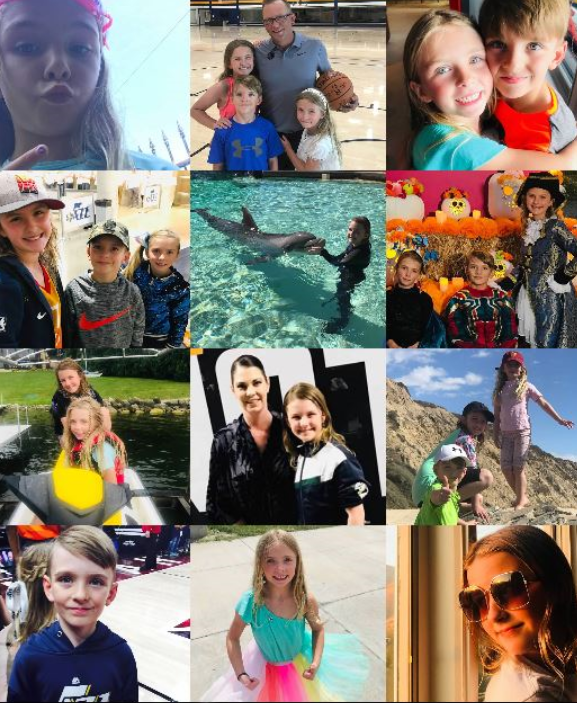
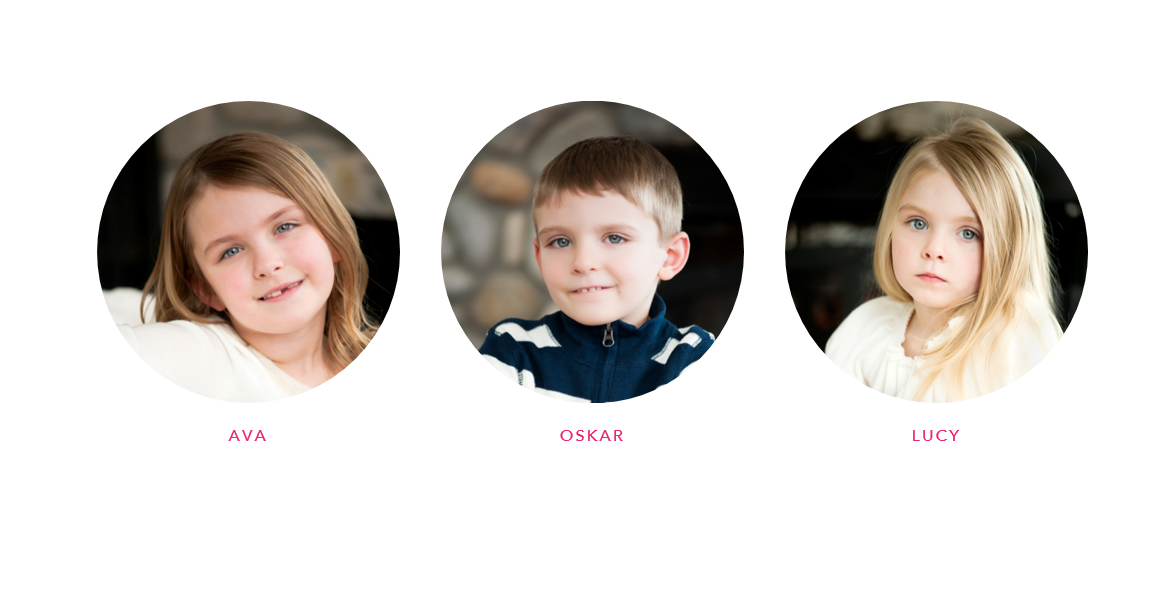 Well, here are our three children. We didn’t get to have the fourth child we planned on having to complete our family. We were told by our genetic counselors that it would be “irresponsible” to have a fourth child when you know you have three children with an undiagnosed genetic dysfunction. I guess it wasn’t in God’s plan.
Well, here are our three children. We didn’t get to have the fourth child we planned on having to complete our family. We were told by our genetic counselors that it would be “irresponsible” to have a fourth child when you know you have three children with an undiagnosed genetic dysfunction. I guess it wasn’t in God’s plan.
I mourn the loss of the fourth child every day.
We did not get the house with the white picket fence either.
Ava is now eleven years old. Oskar is now nine years old. And, Lucy is now seven years old.
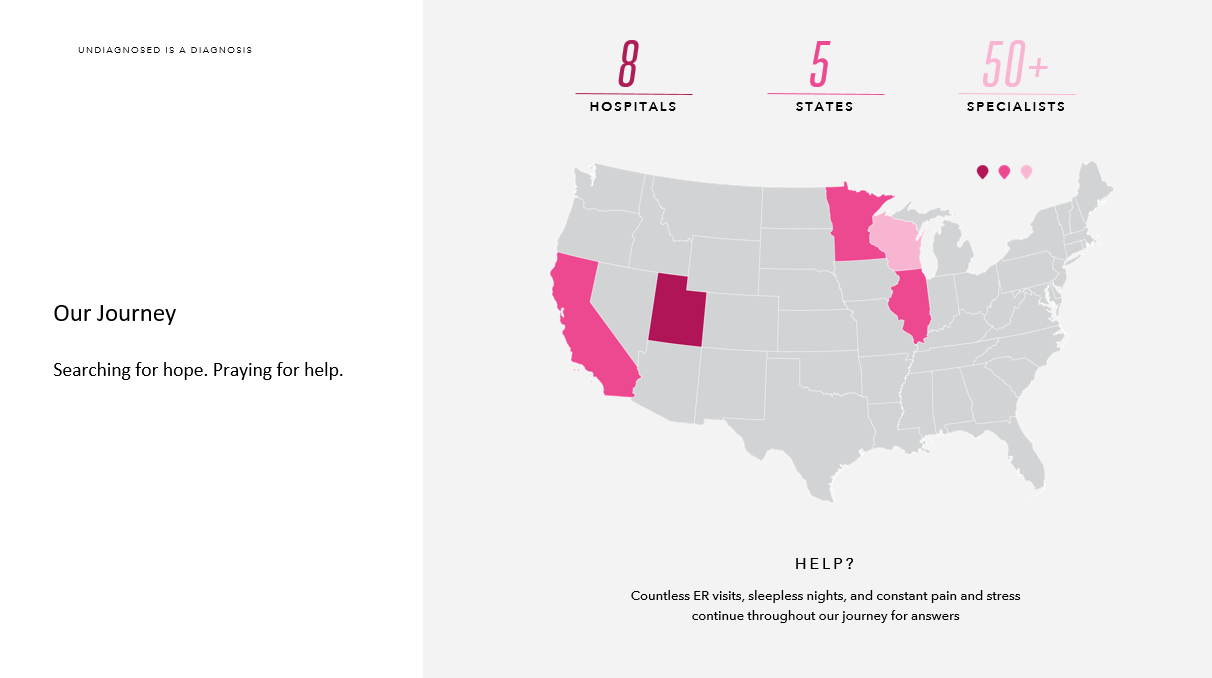
We have been to eight hospitals in five different states. We have seen over fifty specialists. And, we still do not have answers for the root cause of our children’s health concerns. Similar to many rare and undiagnosed families, we have had countless emergency room visits, hospital admittance and even lived at the hospital for six weeks. This is nothing compared to the many families living in hospitals around the world. I will not complain about six weeks.
 Our journey started with Ava. Ava was born healthy.
Our journey started with Ava. Ava was born healthy.
When she was three, Ava had a bump on her head. I went to my pediatrician several times. He finally agreed to send me to a neurologist. Dr. John Ruge, our neurologist, ordered a MRI right away. Ava had a large arachnoid cyst.
This was my introduction into learning that my baby girl was not “perfectly healthy.” This was a wakeup call. The news rocked my world back then. I remember being so scared. I remember the neurologist telling me that she should not play “ball” sports. No gymnastic. No horseback riding, etc. I remember thinking how much Ava was going to miss out in life. I thought that was such a big deal. I was so naive. I wish I could go back to where Ava “just” had an arachnoid cyst. Little did I know that Ava was eventually going to enter into the depths of hell? Real pain.
In the fall of 2012, Ava started to have different symptoms. Her hands turned red. The redness spread throughout her limbs and her head started to hurt. Temperature (heat and cold) started to affect her. Fatigue was playing a role now. And, she had “mast cell like” rashes that started. Her head started to hurt more. We decided to take her to a different hospital in Chicago for a second opinion.
Ava started in rheumatology. They sent us to dermatology. They sent us to neurology. We ended up getting the diagnosis of “unknown” and she told me to read a book written by a mother living with a son that is undiagnosed. I never knew before this moment that a child could be Undiagnosed. I must have been really naive. I thought doctors did not stop until they had a diagnosis for their patient. I remember screaming crying on the floor one night at God and saying, “What are we supposed to do now?!”
The answer came back as DO NOT stop looking for a diagnosis. Move on to the next hospital. Move on to the next specialist. And, off we went…
The next stop for Ava was the Mayo Clinic in Rochester, MN. I remember the specialist saying, “You never want to be interesting to doctors. And, Ava is fascinating!” We have heard that so many times with our children and with me. It’s not something to brag about. Dr. Phil Fischer diagnosed Ava as having an “unknown autonomic neuropathy.”
During this time, we tested our house for everything from mold to meth. We were in a panic that there could be something in the house doing this to our children. It was a dead end too.
The next stage of our lives takes us off the “autonomic train ride” for a few months.
At the age of five, Ava was cleared by her neurosurgeon for her arachnoid cyst. The arachnoid cyst was “happy neighbors” with her brain. The neurologist cleared her and said to come back in three years.
Unfortunately, everything changed dramatically for Ava. She hit her head. And, she started to have horrible headaches. The word “horrible” doesn’t do it justice. She screamed like a wild animal. She could not function. She would sit on her pink beanbag all day and scream all night. We took her to the ER several times before we fought and received a repeat MRI. It did not show any changes from the previous MRI. Everything was stable. They accepted that her headaches were from hitting her head and labeled her headaches as coming from a post-traumatic concussion.
Ava continues to scream in pain every single day and night. I took her to about five different specialists within neurology. The pain came in waves. When we were in the ER, her head didn’t hurt every second. So, when the doctor came in and didn’t hear her screaming, they didn’t listen to me. I tried to tell them that she screams all night and they still didn’t believe me.
More ER visits and two more different hospitals, no one rescanned her and no one truly believed us. My husband started attending all of the appointments and the ER visits. The doctors still didn’t listen. There is documentation in the notes from the second to last ER visit. “No further scans needed.” We were sent home on Tylenol.
A few days later, I put Ava in the car for yet another long drive to a fifth hospital. I called my husband and told him to meet me in Wisconsin. He said, “I will be there.”
Ava was in so much pain. The ER doctor called for a neuro consult. They came down and said that they would see her next week. This was a Thursday. No way. My husband and I refused to leave. Thankfully, the ER doctor agreed to keep us on the basis of her pain level. In the moments that followed, Ava started to complain that she couldn’t see and that her spine in her neck was hurting. She had papilledema and it later turned out her spinal pressure was 55, normal is 20. She was about to go blind and death would have been knocking on her door.
 Ava had a subdural hygroma. She ended up having four cranial surgeries: two external drains, one arachnoid cyst fenestration that didn’t work and is now shunt dependent. We still do not know if this was caused by a rupture of her arachnoid cyst or by whatever unknown is going on in her body. Ava is still Undiagnosed. She still gets the strange rashes. She now has been diagnosed with Eosinophilic Esophagitis (EOE), motility disorder, anxiety, temperature intolerance, dysautonomia, autonomic neuropathy and small fiber polyneuropathy plus many more…
Ava had a subdural hygroma. She ended up having four cranial surgeries: two external drains, one arachnoid cyst fenestration that didn’t work and is now shunt dependent. We still do not know if this was caused by a rupture of her arachnoid cyst or by whatever unknown is going on in her body. Ava is still Undiagnosed. She still gets the strange rashes. She now has been diagnosed with Eosinophilic Esophagitis (EOE), motility disorder, anxiety, temperature intolerance, dysautonomia, autonomic neuropathy and small fiber polyneuropathy plus many more…
Recently, we did a followup MRI. Ava still has her Arachnoid cyst, subdural hygroma and shunt. In addition, she has a subdural hematoma. Our neurologist emailed our neurosurgeon and asked how to handle since there is no protocol.
Since Ava is asymptomatic for headaches, he decided to do nothing. It’s a waiting game and we pray she stays asymptomatic. For Ava to have an arachnoid cyst, subdural hygroma and a subdural hematoma and to be cognitively perfect, she is a miracle child.
We are very blessed to have Ava here with us today. However, her issues inside of her head are only a part of her journey. Ava’s autonomic neuropathy causes her shoulders, tummy, chest, head, legs, and arms to hurt every single day. She battles extreme fatigue. We treat her with distraction. No drugs. Just distraction. She has missed a tremendous amount of school this year. We have started to accept that this extreme fatigue may be her new normal.
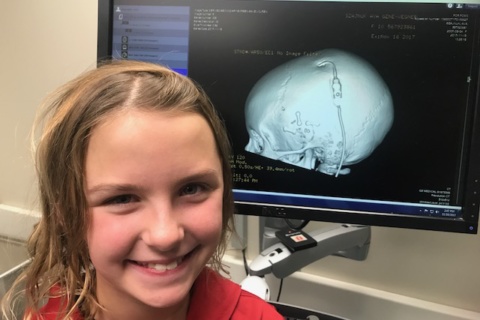 Ava in the ER for a CT scan
Ava in the ER for a CT scan
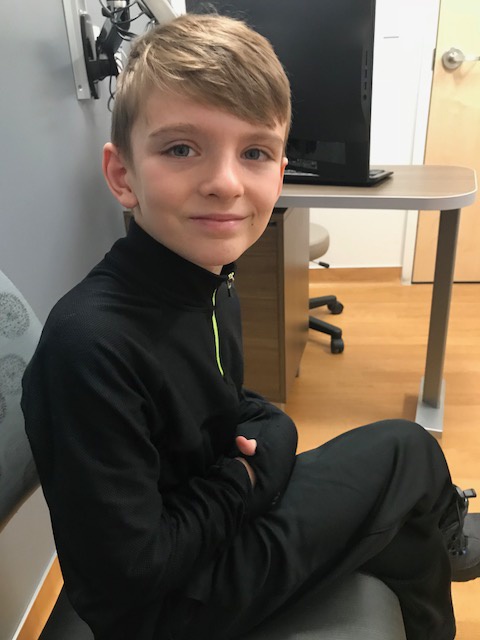
Now on to OSKAR
 After finding out Ava had an arachnoid cyst, Oskar starting having issues. We had a work up done in Chicago for fatigue, leg pain, low-grade fever, and many other symptoms. Oskar started in infectious diseases. They sent us to at least five other specialties. We ended up in oncology. The fear was leukemia. When it wasn’t leukemia, they were at a dead end. I remember the doctor telling me after months of tests on Oskar and many appointments that they just did not know what to do next. When I mentioned that we were told that Ava had an autonomic neuropathy, the infectious disease specialist said, “Well, I would follow that trail with Oskar. We have no idea what to do next. I would go to Mayo with Oskar.”
After finding out Ava had an arachnoid cyst, Oskar starting having issues. We had a work up done in Chicago for fatigue, leg pain, low-grade fever, and many other symptoms. Oskar started in infectious diseases. They sent us to at least five other specialties. We ended up in oncology. The fear was leukemia. When it wasn’t leukemia, they were at a dead end. I remember the doctor telling me after months of tests on Oskar and many appointments that they just did not know what to do next. When I mentioned that we were told that Ava had an autonomic neuropathy, the infectious disease specialist said, “Well, I would follow that trail with Oskar. We have no idea what to do next. I would go to Mayo with Oskar.”
 We went back to the Mayo Clinic now with both Oskar and Ava, where she was currently being treated for her autonomic neuropathy. During the visit with Dr. Fischer, he was even more fascinated that there were two of them. Oskar even had epinephrine levels so high that the NIH did not know what to make of it. We spent more time traveling six hours each way in the car and staying in hotels for yet another workup on Oskar.
We went back to the Mayo Clinic now with both Oskar and Ava, where she was currently being treated for her autonomic neuropathy. During the visit with Dr. Fischer, he was even more fascinated that there were two of them. Oskar even had epinephrine levels so high that the NIH did not know what to make of it. We spent more time traveling six hours each way in the car and staying in hotels for yet another workup on Oskar.
It always comes back to Ava. With Ava’s trauma, we were off the trail for Oskar for about a year. I feel deeply guilty for stopping Oskar’s fight for answers. I didn’t have a choice at the time. I had to focus on Ava. When we moved to Utah and I started back up to find answers for Oskar, I was confronted by a specialist. She scolded me for grouping the kids together. She told me that Oskar and Lucy need to be looked at without talking about Ava. How was I to explain why I stopped appointments for Oskar without telling Ava’s story? Of course, she made me cry. She was right. I have to focus on Oskar now. I have to focus on Ava and on Oskar. Oskar is diagnosed with an Undiagnosed genetic dysfunction. An unknown autonomic neuropathy. He has had countless exams, procedures and still no answers. We treat his symptoms as best as we can. He definitely has a motility disorder, unexplained fatigue, temperature intolerance and many more issues. Oskar lives with pain and fatigue every single day like Ava but he continues to be a sweet and funny little boy. Oskar missed over fifty percent of his 1st & 2nd grade year due to his pain. He is currently attending a little more school this year as he is learning he needs to push through his pain.
Now on to Lucy
 I feel like I missed an entire year of Lucy’s milestones. Lucy started showing similar symptoms in the spring of 2013. Fatigue, redness, pain in her hands, legs, feet and her tummy.
I feel like I missed an entire year of Lucy’s milestones. Lucy started showing similar symptoms in the spring of 2013. Fatigue, redness, pain in her hands, legs, feet and her tummy.
So now, we were off the charts on the “interesting” scale. We had three children with a suspected autonomic neuropathy, genetic dysfunction. Doctors still did not know how to treat the their symptoms.
When I take a second to look back everything, I feel like we skipped a lot of the “normal” doctor appointments that parents have for their children. We were escalated up the ladder so quickly with the autonomic neuropathy. We had to go back and start over with Lucy…and with Oskar. The children needed to see an ENT, sleep studies, etc. In the two last years, we have found out that Lucy has central sleep apnea, she had her adenoids and tonsils out. There were issues we were ignoring due to the focus on finding answers in the big scheme of things. There are so many different parts of the body to focus on and so many different specialists to see for each body part. It is exhausting to have one child needing to see many different specialists. It is not realistic to be doing it for three children in the current medical system now.
 In the last two years, Lucy has been to the ER seven times and admitted three. A simple virus can take her down. A simple dog bite on Oskar’s soccer field took her down. Since there are no other children like mine, there is no protocol. Thanks to Dr, John Carey, we now have a letter stating our history as a family. When we were in Madison this past Christmas, Lucy became ill. I asked her what was wrong. She wanted to get something to scratch her throat. I opened her mouth and looked with a flashlight. It was horrifying to see inside her mouth. As it spread across her entire body, we realized it wasn’t strep or hand, foot, and mouth disease. It was something different. When we arrived at the ER, the doctor read Dr. John Carey’s letter and it gave me instant credibility, which was priceless. Lucy was admitted and it helped her get an edge on the unknown virus.
In the last two years, Lucy has been to the ER seven times and admitted three. A simple virus can take her down. A simple dog bite on Oskar’s soccer field took her down. Since there are no other children like mine, there is no protocol. Thanks to Dr, John Carey, we now have a letter stating our history as a family. When we were in Madison this past Christmas, Lucy became ill. I asked her what was wrong. She wanted to get something to scratch her throat. I opened her mouth and looked with a flashlight. It was horrifying to see inside her mouth. As it spread across her entire body, we realized it wasn’t strep or hand, foot, and mouth disease. It was something different. When we arrived at the ER, the doctor read Dr. John Carey’s letter and it gave me instant credibility, which was priceless. Lucy was admitted and it helped her get an edge on the unknown virus.
At six years old, Lucy lives in pain every single day. What is her future going to be? This scares me every single day. She even started to lose vision and has been diagnosed with abdominal migraines with visual complications as well as complex migraines. She is four!?! A few weeks ago, she couldn’t walk for a few days. We took her into the ER again and she had X-rays taken of her legs. The bone structure of her legs were perfect. Why couldn’t she walk? The doctor in the ER felt strongly that it was from her unknown autonomic neuropathy. It is not easy to watch my youngest suffer in pain.

Now on to my journey
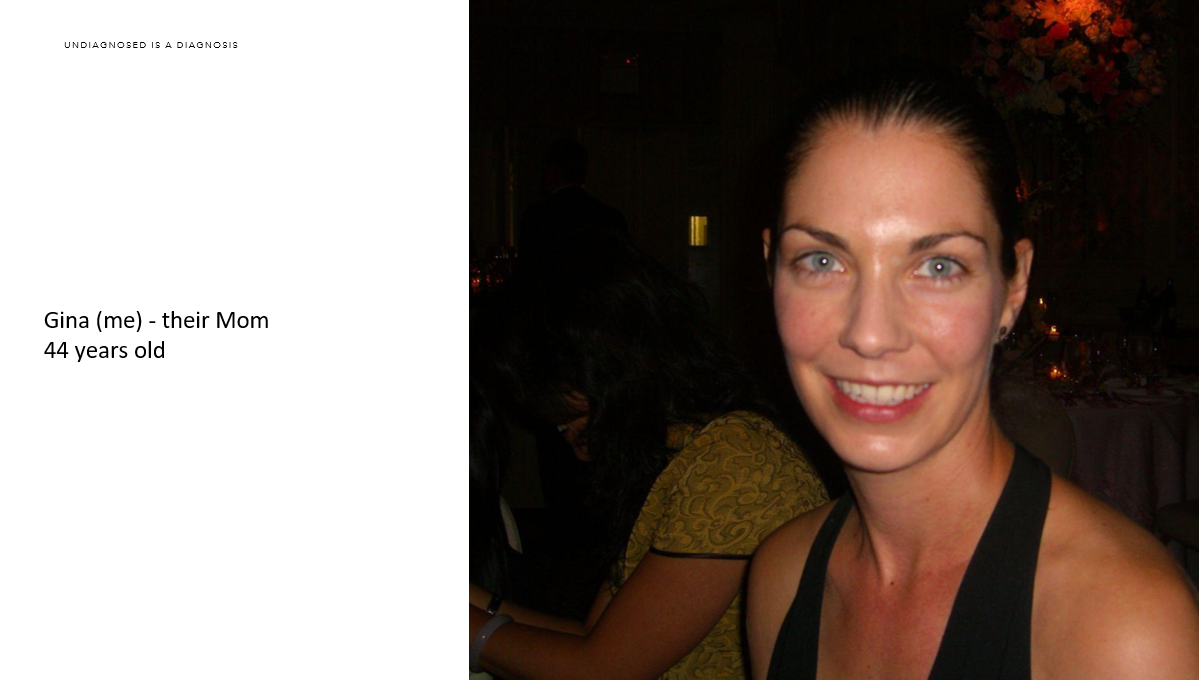
I am now 46 years old and still suffer daily
As I mentioned earlier, I am undiagnosed. It has been an extremely exhausting journey with my children’s diagnostic odyssey in addition to mine.
 I started having issues when I gave birth to Ava. I was “on fire” after my c-section. I kept the room so cold Justin got sick. I have been on fire ever since. When Ava’s head trauma and journey through hell happened, my body went to a whole new level of instability. I would check myself into the ER for a panic attack along with Ava for her headaches. I was on lorazepam for a year and a half. My distal joints all popped and I lost the strength in my hands. I felt like I was having a heart attack every single day. During one of Ava’s Mayo Clinic stays, I asked Dr. Fischer if I could have a workup done. He agreed. I saw every specialty and had around a million dollar workup there over about two years. They sent me back to Utah with a diagnosis of undifferentiated connective tissue disease and inflammatory arthritis. The University of Utah disagreed with their diagnoses and have labeled me as undiagnosed with many different issues going on like EOE, aggressive and progressive osteoarthritis, hypertension, intermittent nocturnal hypoxia, sleep apnea and I have myoclonic jerking all night. None of this is normal. I have lots of blood levels off but not in a way that fits with any known diagnosis. Recently, I have had uncontrollable jerking movements during the day. I will be having additional testing in the next few months for a movement disorder. I live in pain every day. I am fine with living in pain as long as I know I’m staying around for many more years.
I started having issues when I gave birth to Ava. I was “on fire” after my c-section. I kept the room so cold Justin got sick. I have been on fire ever since. When Ava’s head trauma and journey through hell happened, my body went to a whole new level of instability. I would check myself into the ER for a panic attack along with Ava for her headaches. I was on lorazepam for a year and a half. My distal joints all popped and I lost the strength in my hands. I felt like I was having a heart attack every single day. During one of Ava’s Mayo Clinic stays, I asked Dr. Fischer if I could have a workup done. He agreed. I saw every specialty and had around a million dollar workup there over about two years. They sent me back to Utah with a diagnosis of undifferentiated connective tissue disease and inflammatory arthritis. The University of Utah disagreed with their diagnoses and have labeled me as undiagnosed with many different issues going on like EOE, aggressive and progressive osteoarthritis, hypertension, intermittent nocturnal hypoxia, sleep apnea and I have myoclonic jerking all night. None of this is normal. I have lots of blood levels off but not in a way that fits with any known diagnosis. Recently, I have had uncontrollable jerking movements during the day. I will be having additional testing in the next few months for a movement disorder. I live in pain every day. I am fine with living in pain as long as I know I’m staying around for many more years.
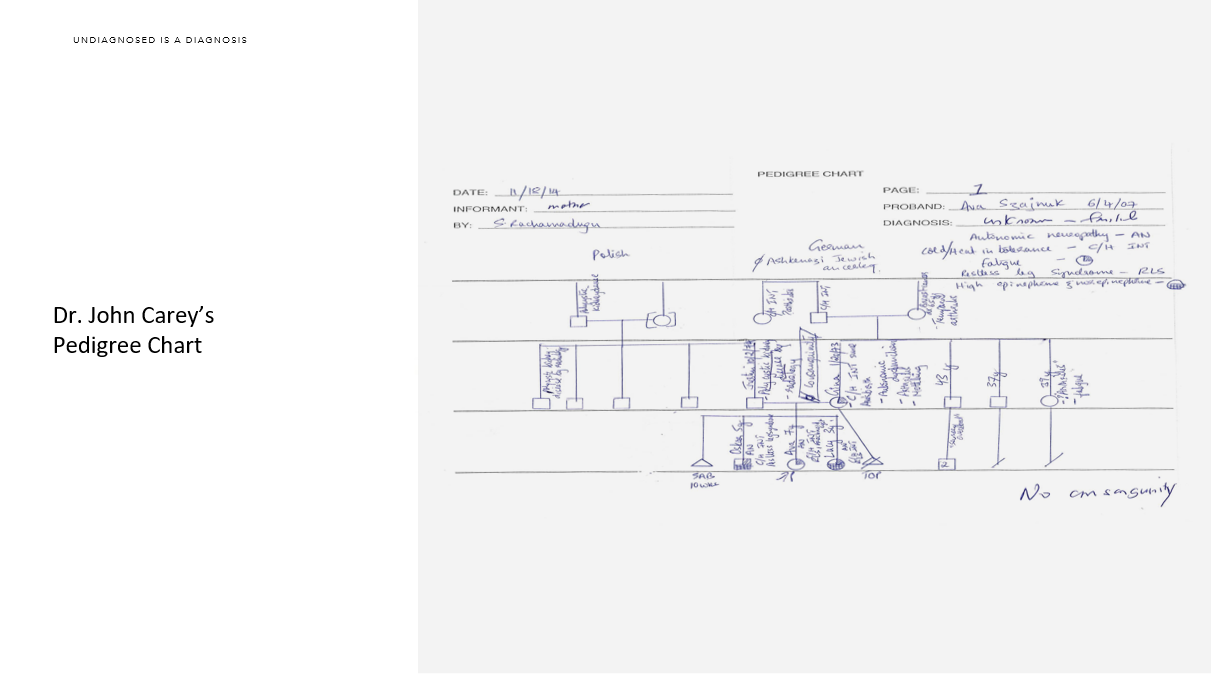
 With all that said, we went out of the four walls of multiple hospitals and into the world of genetics. We started in Wisconsin with Dr. Gunter Scharer and his team, which included Dr. Howard Jacob. We agreed to fight for whole genome sequencing for our family of five in a clinical setting. We all thought we would have a good chance to push on the insurance industry since we had three afflicted children and two generations. I was so naïve back then. I was sure we would get it done. I had a great genetic counselor, Regan. She spent hours and hours working on our three insurance letters.
With all that said, we went out of the four walls of multiple hospitals and into the world of genetics. We started in Wisconsin with Dr. Gunter Scharer and his team, which included Dr. Howard Jacob. We agreed to fight for whole genome sequencing for our family of five in a clinical setting. We all thought we would have a good chance to push on the insurance industry since we had three afflicted children and two generations. I was so naïve back then. I was sure we would get it done. I had a great genetic counselor, Regan. She spent hours and hours working on our three insurance letters.
I remember her saying, “Every day I think I’m done with the letters but then I see new research released that supports whole genome sequencing over whole exome sequencing.”
We were obviously denied. They actually had it in their policy, “At this time the clinical utility of such testing has not been established.”
So, we looked at doing whole genome sequencing with Dr. Jacob through research. Unfortunately, it wasn’t possible for us. The price tag at the time was $30,000, $150,000 for our family of five. When we were discussing all of this with Dr. Jacob, he promised if he did our sequencing that we could “own” our data. We were also in talks with Dr. Stephen Kingsmore at the time about doing whole exome sequencing in a research study. We would not get our data and we would not get our results. We did the research study and we have no idea what the results were of our whole exome sequencing.
However, we continued on with Dr. Jacob and his team. We went for whole exome sequencing through our insurance next. Denied.
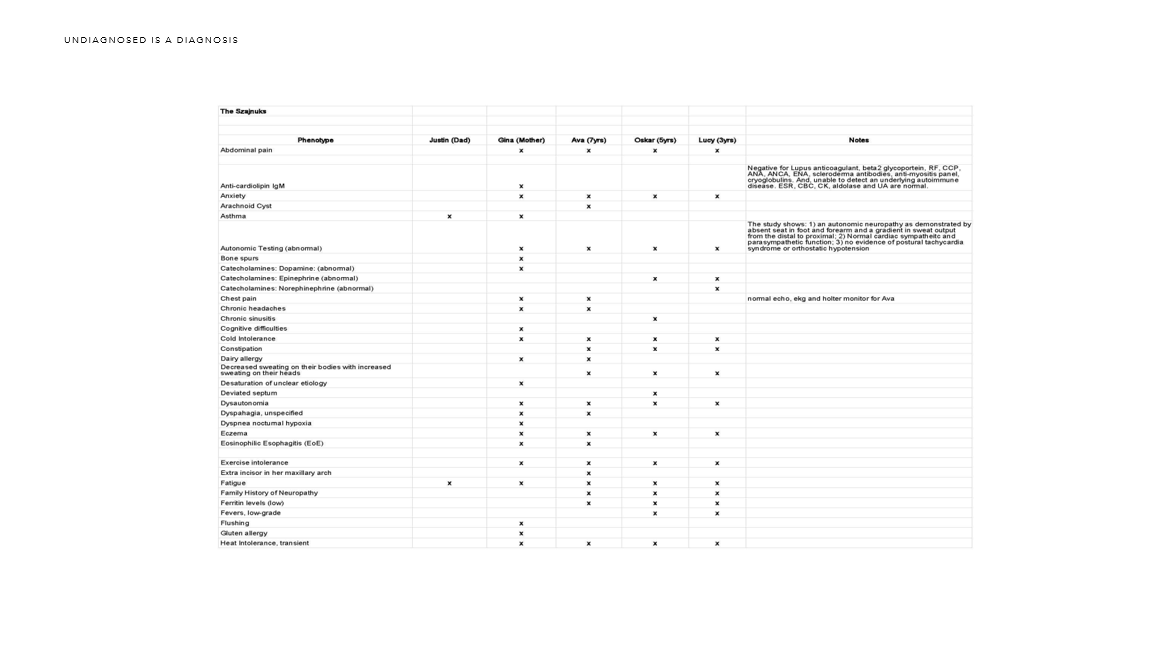
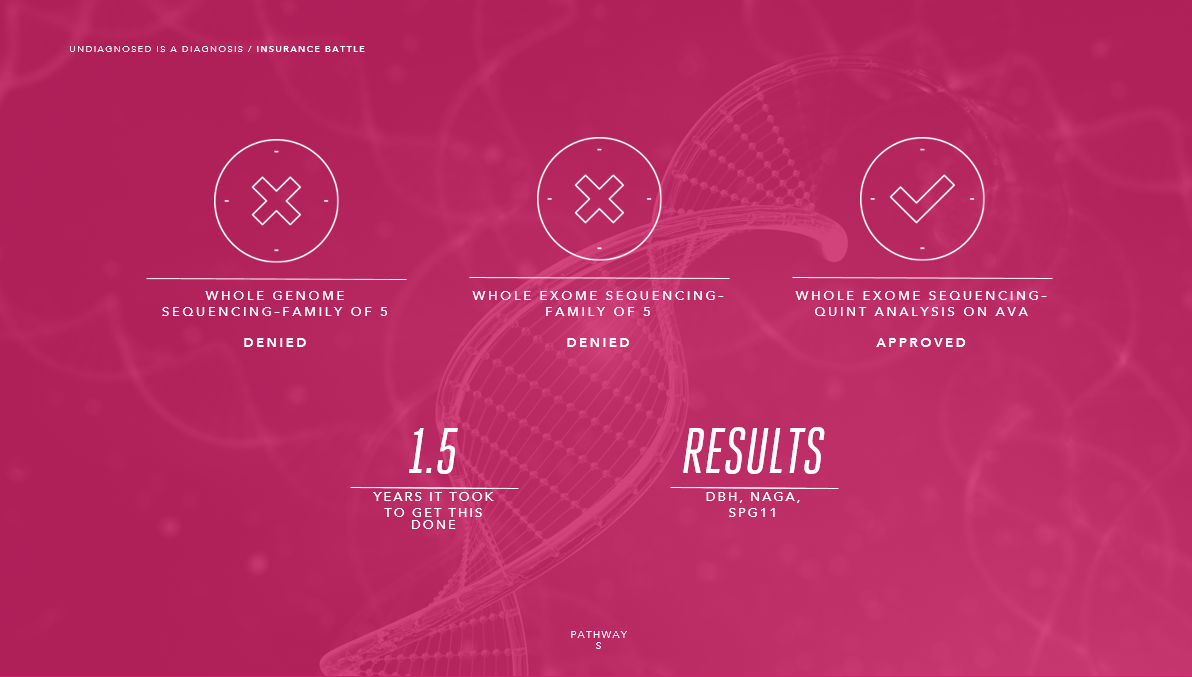 We ended up getting a quint analysis approved for Ava. This meant that we were all sequenced but Ava was the only one analyzed. They found three variants: DBH, NAGA and SPG11. Justin and I flew all the way from Utah back to Wisconsin for the results. We were hoping for better news. Unfortunately, we did not find a diagnosis through whole exome sequencing.
We ended up getting a quint analysis approved for Ava. This meant that we were all sequenced but Ava was the only one analyzed. They found three variants: DBH, NAGA and SPG11. Justin and I flew all the way from Utah back to Wisconsin for the results. We were hoping for better news. Unfortunately, we did not find a diagnosis through whole exome sequencing.
The good news was that I was able to get our data on a hard drive. Thank you to my team at the Human Molecular Genetics Center at MCW for continuing to work with our family and making sure we were able to open and access the data on the hard drive.


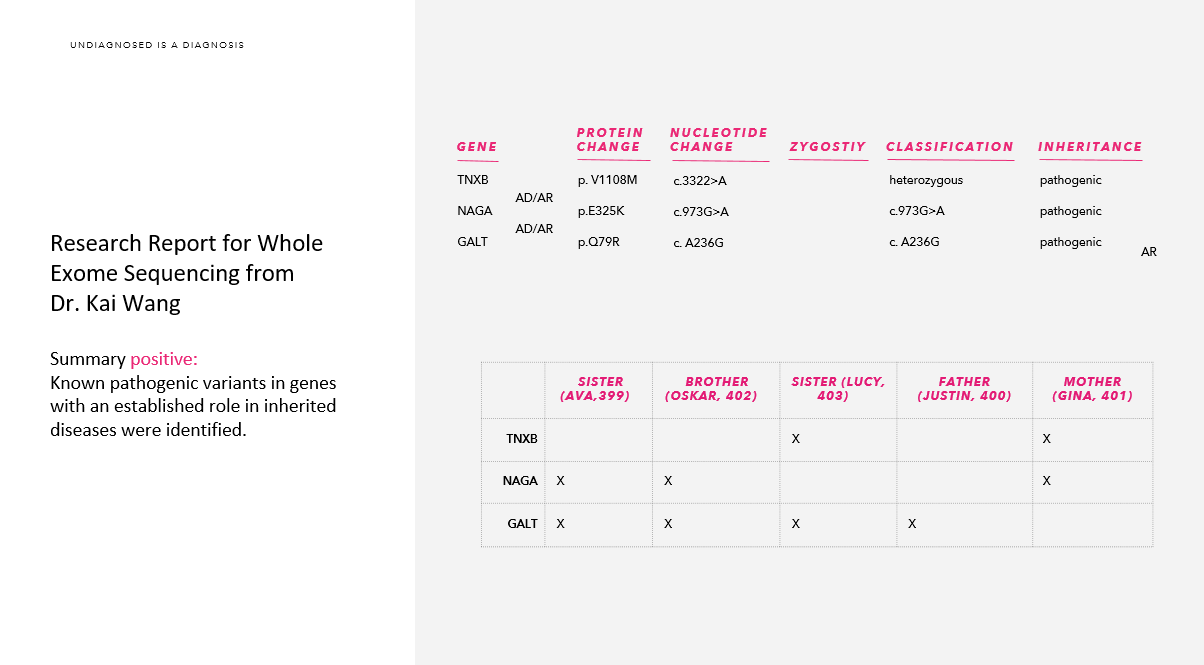 One year ago at the ACMG conference in Salt Lake City, I walked up to the Tute Genomics booth and asked Josh Forsythe and Dr. Reid Robison if they would analyze our data again. Dr. Kai Wang took my hard drive from my purse and uploaded it to his laptop. They couldn’t believe that I was walking around with my USBs in my purse with our raw data on it.
One year ago at the ACMG conference in Salt Lake City, I walked up to the Tute Genomics booth and asked Josh Forsythe and Dr. Reid Robison if they would analyze our data again. Dr. Kai Wang took my hard drive from my purse and uploaded it to his laptop. They couldn’t believe that I was walking around with my USBs in my purse with our raw data on it.
This was to be our second set up eyes on our whole exome sequencing results. I am so thankful to Kai for his time and his devotion to our family. Kai’s report came back with more variants. He analyzed all five of us and not just Ava. We still did not find a solid answer.
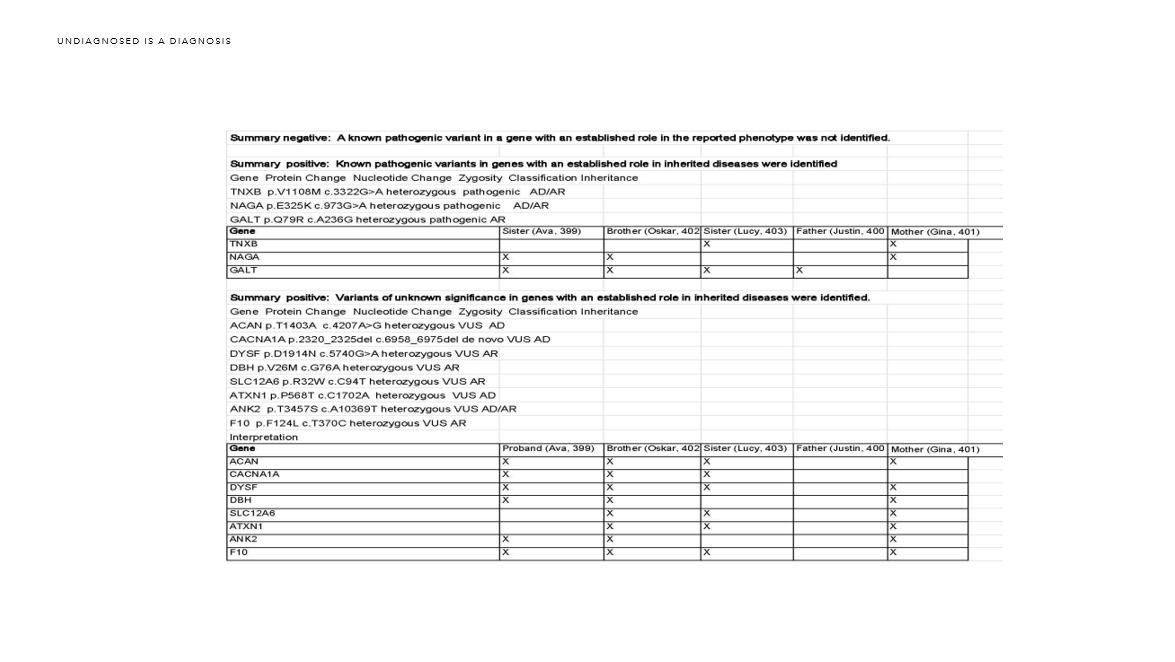
 So, I took those two reports and combined them. I added in our family phenotype and sent the reports and our data on to the Rare Genomics Institute to the program Science 2.0 they were launching. I’m still waiting on their results.
So, I took those two reports and combined them. I added in our family phenotype and sent the reports and our data on to the Rare Genomics Institute to the program Science 2.0 they were launching. I’m still waiting on their results.
 February 29, 2015: From there, I spoke at the Utah Rare 1st Inaugural Symposium last Rare Disease Day. I was invited by Cristina Might, famous in the world of genetics with her husband, Matthew Might, for discovering their son had NGLY1.org. Bertrand Might was the first in the world to be diagnosed for NGLY1. Through sharing our story at the symposium, Cristina and I were asked to have a meeting about the Utah Genome Project and for the University of Utah’s and Intermountain Primary Children’s Hospital’s Undiagnosed Program they want to launch, which is now called “Penelope”. In this conversation, I asked, “Is it possible for my family to have our whole genome sequencing done as well as my parents?”
February 29, 2015: From there, I spoke at the Utah Rare 1st Inaugural Symposium last Rare Disease Day. I was invited by Cristina Might, famous in the world of genetics with her husband, Matthew Might, for discovering their son had NGLY1.org. Bertrand Might was the first in the world to be diagnosed for NGLY1. Through sharing our story at the symposium, Cristina and I were asked to have a meeting about the Utah Genome Project and for the University of Utah’s and Intermountain Primary Children’s Hospital’s Undiagnosed Program they want to launch, which is now called “Penelope”. In this conversation, I asked, “Is it possible for my family to have our whole genome sequencing done as well as my parents?”
They agreed it and we were off to get approval from our geneticist, Dr. John Carey. They wanted to hear from him that this was a genetic issue for our family.They also took our exome data and analyzed it. We are hoping for our results in the next few weeks.
What I have learned from our diagnostic odyssey in the world of genetics is that it is important to have many different eyes on the data.
We also applied to the Undiagnosed Diseases Network (UDN). We are currently in the middle of the application process. They have all of our medical files and images. They will analyze our whole genome again through their machines and through their eyes. However, they are waiting to see if the Utah Genome Project and Dr. John Carey find an answer before they will decide to accept us.
Even if the Utah Genome Project or the UDN do not find an answer for our Undiagnosed genetic dysfunction, at least our data is in their machines. There is new information coming out every single day.
As a mother, I did everything humanly possible to find the answers for my three children. Dr. Carey made it very clear to me that he didn’t want to get my hopes up. I explained that I can sleep better at night knowing that I went all the way until I got the whole genome sequencing done. And, I was able to get my parents done as well. Maybe we will find answers for me? We can only pray.
In the meantime, what is it like to be undiagnosed?
 “To be undiagnosed is like being a child without a “home”.
“To be undiagnosed is like being a child without a “home”.
Not a home in the physical sense, but in the sense of feeling you are without that one place in the world that provides the most comfort. The place that protects you from outside threats, keeps you warm inside, and gives you that safe, confident feeling you have when knowing all of your surroundings.
Far too many children throughout our communities are without this feeling of comfort and confidence.
Millions of children have what is called an “undiagnosed rare disease”, which is a medical condition without a known cause despite great effort to research, discover, and identify the cause through extensive evaluation.
Our children and loved ones deserve better. No child should be left undiagnosed and have to live without feeling comfortable, safe, and confident in knowing their surroundings inside and out. Every child and loved one not only deserves a diagnosis, but they need it – and time is of the essence.
So when someone asks you what “Undiagnosed” means, you can tell them to think about life without a home. Life without full comfort, full warmth, and full confidence in your surroundings.
Living “undiagnosed” is nothing more than living the unknown.”
April 29, 2016: Thank you to Governor Herbert for declaring April 29th, as Undiagnosed Day. It is an honor to have the State of Utah be the first in the history of the United States to have a declaration an Undiagnosed Day.
What is Undiagnosed Day?
Undiagnosed Day is a special day where you can help make millions of children and adults as well as their loved ones living undiagnosed feel a great sense of comfort and confidence in knowing they are not alone in their search for answers.
Undiagnosed Day takes place on April 29th with a single objective:
Raise awareness among the general public and decision-makers about undiagnosed rare diseases and their emotional, physical and financial impact on the lives of the patients and their families.
The campaign targets primarily the general public and also seeks to raise awareness among policy makers, public authorities, industry representatives, researchers, health professionals and anyone who has a genuine interest in undiagnosed diseases and genetics.
Since 80% of rare and undiagnosed diseases have identified genetic origins, it is imperative to raise awareness for the importance of genetics in the diagnostic odyssey of undiagnosed rare disease patients.
About the Undiagnosed Ribbon:
Undiagnosed ribbon was created by Ava Szajnuk. Ava is nine years old and undiagnosed. Since zebras represent the rare community, we envisioned having a zebra ribbon with baby blue and baby pink colors added to it. We continue to be a part of the rare community but we also stand alone. All rare diseases were once undiagnosed.
May 8th, 2016: Update on our Szajnuk’s Diagnostic Odyssey x 4: This week was a very memorable week for our family. Our first meeting regarding the results from our Whole Genome Sequencing (WGS) was this past Friday, May 6th. We met with Dr. John Carey, a professor of Pediatrics at the University of Utah and our geneticist, along with our genetic counselor, Janice, from the Utah Genome Project. I will be explaining more about the results in a few weeks when we receive the final list of genes found through our WGS. However, what I can share today is that we found around fourteen new genes that we know nothing about!?! I am so overwhelmed by the generosity of the University of Utah and the Utah Genome Project for their continued support and care of our family. Dr. Lynn and Debbie Jorde accepted Dr. John Carey’s request to sequence our family of five, plus my parents, in hopes of finding a new Familial Autonomic Neuropathy gene or a Familial Pain Syndrome gene. They have all been extremely supportive and dedicated to finding a gene that could be causing the disease process in our family. There are so many people to thank on the Szajnuk Research Team. Please know that I am forever grateful to each and everyone of you!
Dr. Carey broke it down to me this way:
We have found around fourteen new genes that breakdown into the following two categories:
1) We know nothing about nine of the genes but they are in OMIN, which means we know something but no human disease. No one has studied them.
2) And, around five of the genes we know absolutely nothing about them and they are not even in OMIN
Dr. John Carey stated, “We know the Szajnuk family has something.” Carey said that the genome sequencing results have offered some clues but there is a lot more work to be done. For more on the Szajnuk’s journey, please watch Fox 13 News Interview on Undiagnosed Day from #UndiagnosedDay on April 29th.
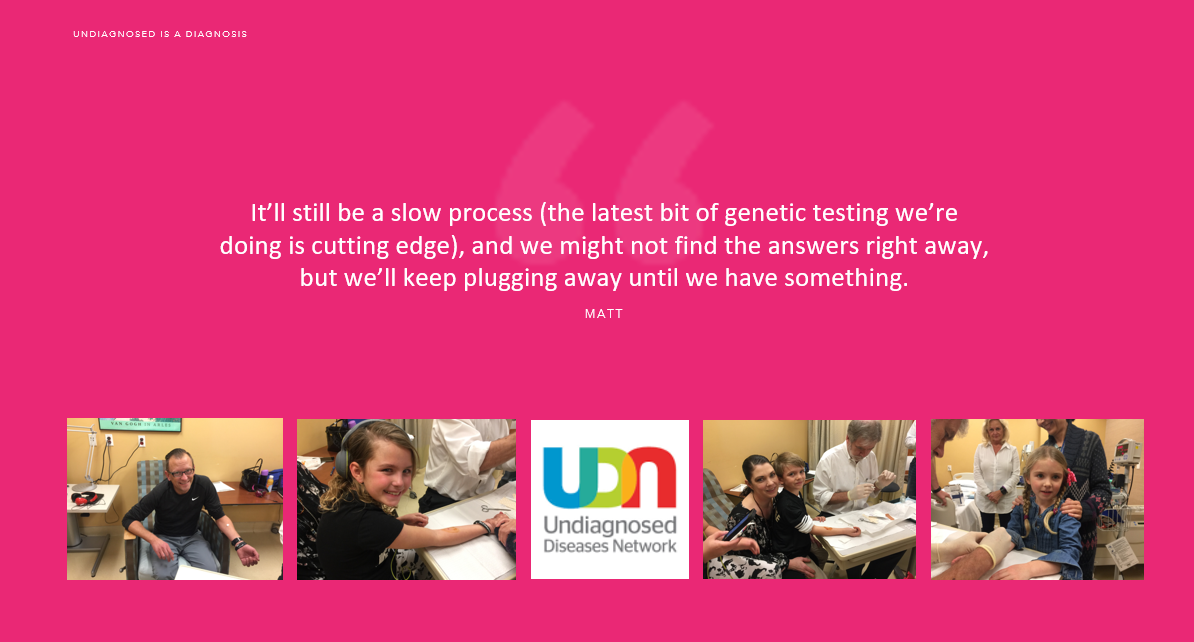
May 8th, 2016: Another update on our journey is that we received the official news on Thursday evening that we have been accepted into the Undiagnosed Disease Network (UDN). The relief and celebration came that night because they not only accepted Ava, they accepted all four of us individually! Ava, Oskar, Lucy and Gina (me)! were all accepted into the UDN. Words cannot express how much this means to our family. The UDN will be collaborating with Dr. John Carey and the Utah Genome project. We will be traveling to Los Angeles to the UCLA Human Genetics (Undiagnosed Diseases Network) to have clinical care for all four of us at the same time. I am so very thankful to everyone involved in making the decision to accept all four of us!
“The UDN Case Review Committee met today and decided to accept Ava, Oskar, Lucy, and your applications into the Undiagnosed Diseases Network! I’ll be sending formal letters of acceptance to you and your referring physician by early next week, but I wanted to let you know ahead of time. -Matt”
When I asked my contact at the UDN if they have ever accepted a family of four, he said, “I don’t think we’ve had a family of four apply since we’ve launched in September.” If you are an Undiagnosed family, please all apply individually!
May 9th, 2016: We also had Andrew Scholte accepted into the New York City Marathon this past week! Congrats! Andrew is on the the Running4Rare team that came together for the first time as an independent entity working with the National Organization of Rare Disorders (NORD) and the Undiagnosed Diseases Network (UDN). Andrew is running for our family as well as all of the Rare and Undiagnosed community. This was a huge gift this week as well!
May 10, 2016: We now have our third WES report from the Science 2.0 program at the Rare Genomics Institute.
Thank you to everyone at the Rare Genomics Institute for all of your hard work and dedication to our family.
Words cannot express how much we appreciate everything you do for all of the Rare and Undiagnosed families desperately trying to find answers. – Gina
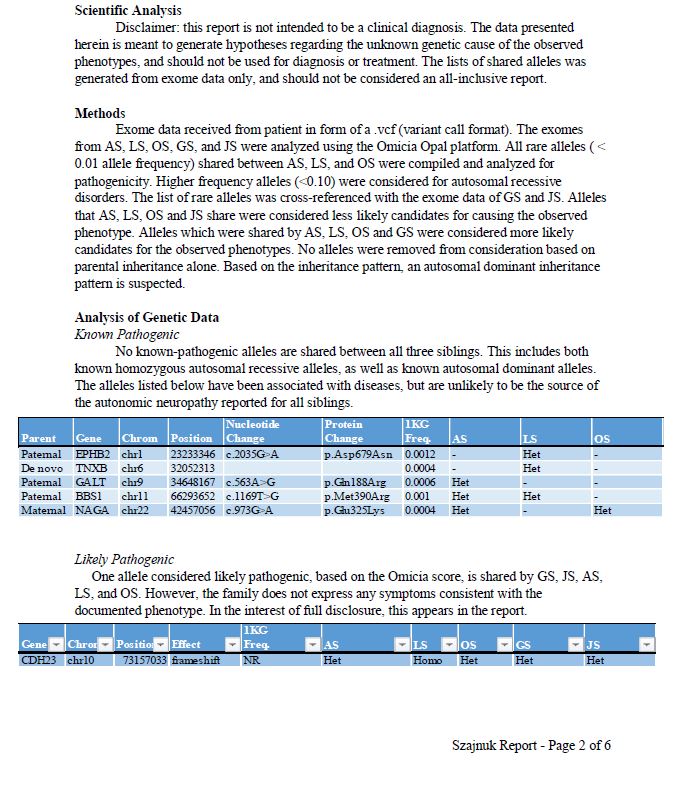
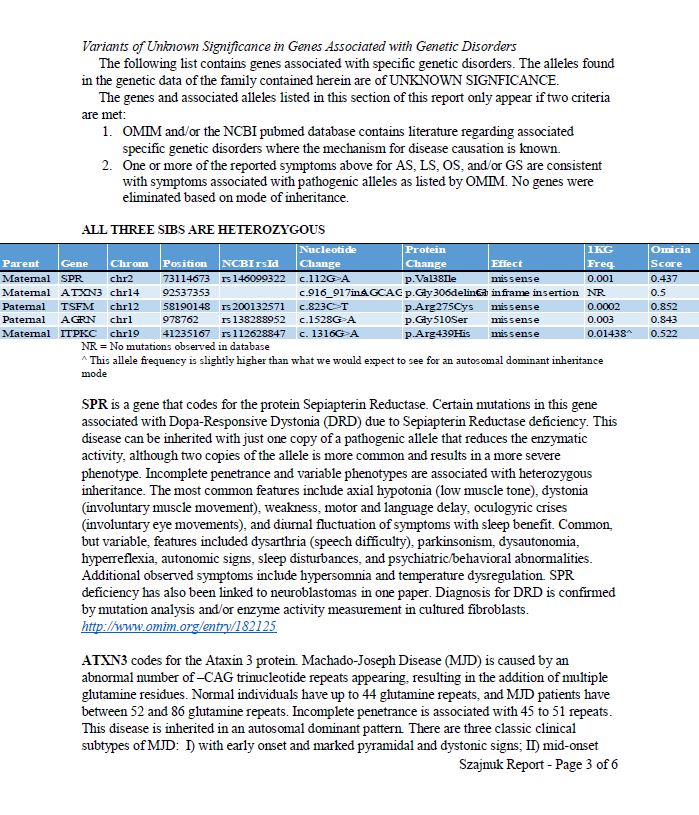
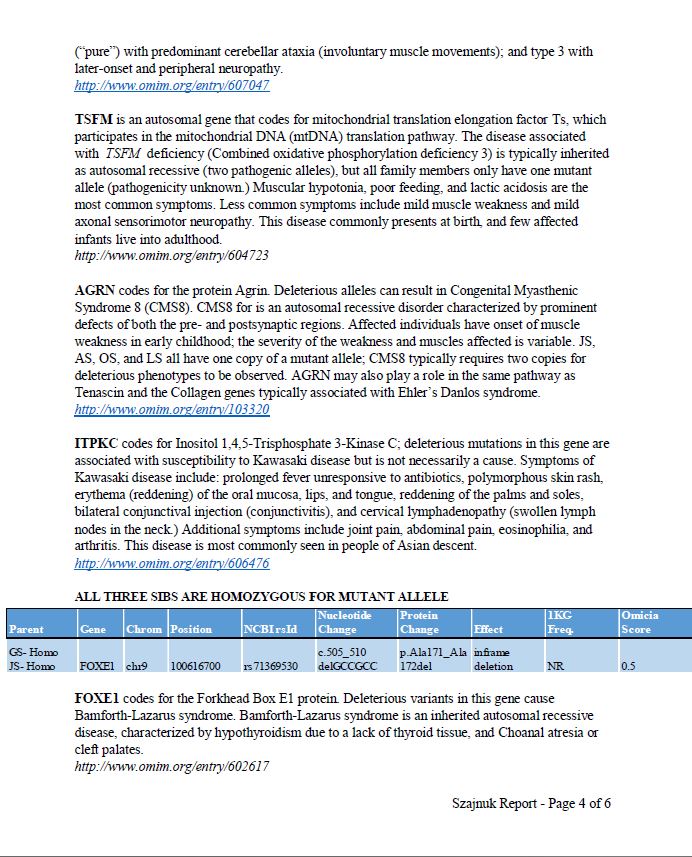
The Szajnuk’s Report:
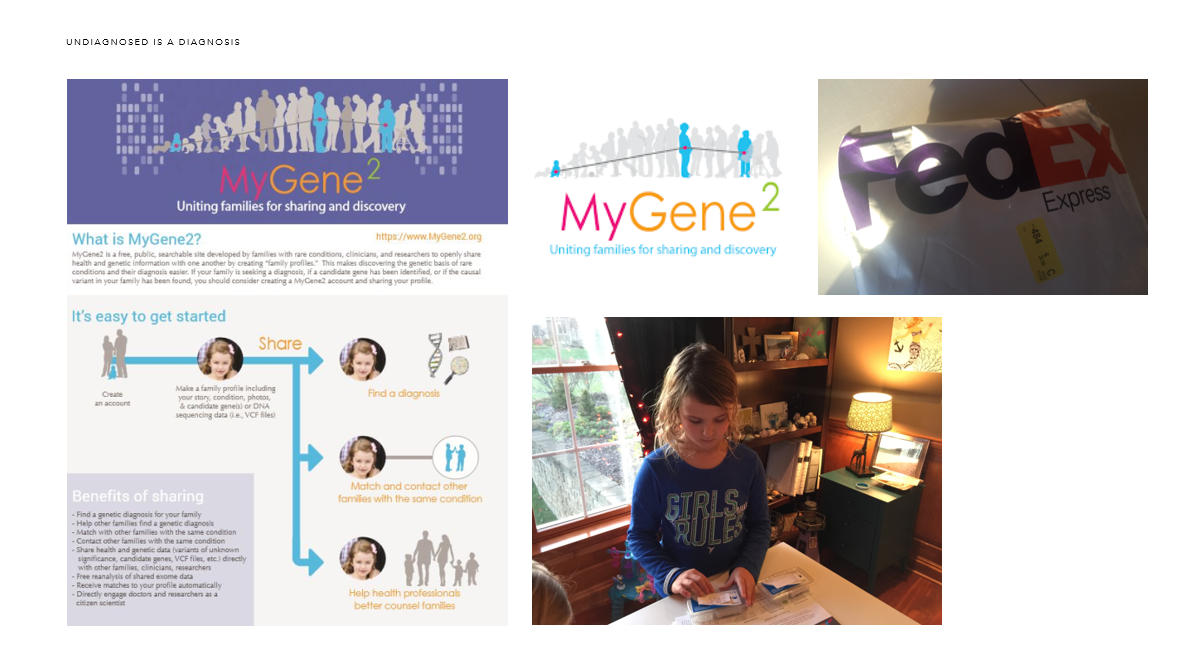
May 10th, 2016: We are also working with MyGene2.org. We have our Whole Exome Sequencing data in their database. We were the first family to upload our data into their site. I was working directly with the MyGene2 Project Leaders, Jessica Chong and Mike Bamshad.
“MyGene2 is a portal through which families with rare genetic conditions who are interested in sharing their health and genetic information can connect with other families, clinicians, and researchers. The genetic cause of most rare conditions is unknown and as a result, most families who undergo exome sequencing or whole genome sequencing do not receive a diagnosis. By sharing information through MyGene2, a family can help and even participate in the discovery of new genetic conditions and the genes underlying these conditions.
Families with rare genetic conditions may use MyGene2 to search for and contact other families who have the same condition or mutations in the same gene in order to share information and offer support. Families have the option to make the information they submit to MyGene2 available to anyone visiting the site (i.e., public) or available to only registered users who have also contributed data to MyGene2. Families also have the choice of whether or not they want to be contacted by clinicians and researchers or other families.
Clinicians who have evaluated families with rare conditions may use MyGene2 to identify and contact families with the same rare condition and / or candidate gene.
Researchers studying a gene or families with a rare condition may use MyGene2 to identify and contact other families who have the same rare condition or candidate gene.”
June 9th, 2016: With the official announcement today, BUCKS NAME JUSTIN ZANIK ASSISTANT GENERAL MANAGER, we will now be moving from Utah to Wisconsin this month. It is an incredible opportunity for our family and we are so excited to move home. I was raised in Madison, WI. I went to college at the University of Wisconsin – Madison. My parents still live in the same house I grew up in on Lake Monona. However, Utah was our home for three years as we were very committed to the community and to the Utah Jazz. It is with heavy hearts that we make this move right now. I will continue to support my RUN families in Utah and Anne Bruns will now be the 2017 Utah Rare Chair.
June 12th, 2016: As I now think to the next chapter in our lives, I am exhausted at thinking about the medical situation and starting all over again. We have moved from state to state but we have also moved from hospital to hospital. This move only exaggerates the need for our specialists to work together…across state lines. We are familiar with our new home hospital from our summer spent there with Ava’s four cranial surgeries as well as our Autonomic Neuropathy specialists. However, we have to start over with every other specialists. I have a Neurologist there but I have to start over with every other specialty too. I met with several of my specialists in Utah and begged them to keep me and I told them I will fly back to Utah for my care. Is this financially realistic? I do not know. I’m just overwhelmed with thinking of starting all over again. Part of me just wants to throw in the towel since we are still undiagnosed. However, I know I cannot and should not do it. I have to have medical care for all four of us.
So, once we get unpacked in early July, my next assignment is starting to find specialists for all four of us in Wisconsin. Exhausting. Truly exhausting.
On a positive note, our fabulous geneticist, Dr. John Carey, will be staying on our Whole Genome Sequencing case along with the head of the Szajnuk’s research team, Barry Moore. And even better news, the Utah Genome Project has agreed to give us our hard drive with all of our data!! Thank you Dr. Lynne and Debbie Jorde! This is huge for our family and it will allow us to have more collaboration. We have already discussed sharing/collaborating with the Undiagnosed Diseases Network (UDN) at UCLA, with the University of Washington and with our team in Wisconsin. I’m hoping that Dr. Howard Jacob also agrees to collaborate as he was the first person involved with our WGS years ago. This is so very exciting to have more eyes on our data and the expertise of all of these incredible people. Dr. Mike Bamshad, Jessica Wang, Jamie Wendt, Matthew Hertzog and the list goes on. Barry Moore and I met last week. We both agreed, “Imagine what the conference call would be like with this group of gifted people all focusing on finding an answer for our family?!?!” It has always been my mission to have collaboration on our WGS. And now, it is actually going to happen!
We will find out the list of genes from Dr. John Carey in the next week or so…
When we do get this list from him, MyGene2 will both help us search for other families out there with the same genes/phenotypes. We also want to get other children with similar phenotype sequenced. I have already suggested Rachel Nielson, Hailey Sampsel, Lashay Hamblin, Brittany Stangley, Katie Petersen and many more as they are all very similar to our children with the digestion issues and/or headaches. We still believe that our children are pre- POTS, (postural orthostatic tachycardia syndrome).
October 29th, 2016: The Undiagnosed Disease Network International (UDNI): Dr. William Gahl invited me to their next meeting in Toyko when NORD/RUN presented on a call with the Undiagnosed Disease Network (UDN) Steering Committee a few months ago. It was a defining moment for me as it was such an honor to be invited! It was a moment I will remember forever. I had my airplane ticket booked immediately! Unfortunately, I am not able to attend now. I am so disappointed as my advocacy work for the undiagnosed rare disease community is so important to me, to my family and to my RUN family. I will keep up to date on what they are doing to move this forward through my relationship with NORD as their Undiagnosed Advocacy Ambassador. This is an incredible document that address the undiagnosed rare disease patient and the UDNI’s recommendations. This is huge for our undiagnosed rare disease community.
November 9, 2016:
We launched the WisconsinRare.org website today!! I am so excited to be working with the incredible and inspiring families here in Wisconsin!
November 10, 2016: I am writing an update today for the first time in a few months. There is so much that has happened these past few months.
We have yet to receive our list of genes from the Utah Genome Project. Due to the IRB, Dr. John Carey is only able to give us the names of the genes verbally. We hope to have the conversation with him soon.
The Undiagnosed Disease Network (UDN) has received the data from the Utah Genome Project and is analyzing our whole genome sequencing data right now. We are scheduled to travel to Los Angeles in December for our UDN visit. The visit is for all four of us – Ava, Oskar, Lucy and me. We are very excited to meet with the team at the UCLA Human Genetics. Justin as well as his mother and father-in-law will be with us as this will be an intense week of procedures and appointments.
The incredible team at MyGene2.com will also be analyzing the data from the Utah Genome Project. However, they also cannot give us our data and can only share their results back to the Utah Genome Project per the IRB. So, MyGene2 has also agreed to do our whole genome sequencing on their own!! They mailed us our saliva kits and we will be mailing them back in the next day or so.
We are so very blessed to have our whole genome sequenced by three different institutions this year. This is a huge step forward for our family. Although we may not have an answer through all of this, I feel like all of my advocacy work and dedication to my mission is helping to open doors for our family as well as many of my RUN families. I am working on getting other RUN families sequenced by MyGene2 as well as to get more families into the UDN program.
I just met with the Undiagnosed and Rare Disease Program at the Children’s Hospital of Wisconsin. They are the ones we started with three years ago when Ava was hospitalized during the summer of 2013. Now that we are back in Wisconsin, the Children’s Hospital of Wisconsin will be our home hospital. This is an incredible and wonderful circle because they saved Ava’s life in 2013. I met the head of the program, Dr. Robert Kliegman. We had a very enjoyable conversation about whole genome sequencing and the need for it to be in clinical setting paid for by the insurance companies. This continues to be a struggle and it should not be. I asked him if he had a choice between ordering whole exome sequencing for a patient or whole genome sequencing, which would he choose? He said that he would choose WGS every time. It is currently not covered by insurance companies as they continue to claim that whole genome sequencing is for research only. This is such a frustrating fight to have with the insurance companies as WGS is crucial in the diagnostic odyssey. We need to continue to push on the insurance industry to recognize that the cost for WGS has dropped and the cost for a diagnostic odyssey is astronomical.
Dr. Kliegman emailed me the next morning and offered to reanalyze our family! I will be dropping off all of our medical files from the past three years to their office tomorrow. We will be working with his incredible team again now in 2016! It is an honor to be a part of this program again and I look forward to meeting with them soon!
We continue to be diagnosed as undiagnosed.
December 8th, 2016:
This is a special time of year for holiday fun. This is a time for making gingerbread houses with your classmates and attending your children’s holiday concerts. Unfortunately, we will miss those holiday activities next week. As most people are running around holiday shopping and preparing for Christmas, our family will be praying for a Christmas Miracle – a diagnosis, treatment & cure. We leave for our Undiagnosed Diseases Network (UDN) visit this Sunday, December 11th. We have been waiting months for our UDN visit. We will be flying to Los Angeles to meet with their UCLA Human Genetics team. We feel so very blessed to have been accepted as we know there are families that have not been accepted.
We have had so many different medical teams and researchers across the country working on our family over the last few years. We have truly been blessed to work with each and every single one of them. They have dedicated so much time and energy into trying to solve our medical mystery of the four of us – Ava, Oskar, Lucy and me. This has been such an emotional and physical journey with major financial consequences. We owe so much to everyone that has supported us within the medical community, our family, our friends and everyone within the rare community.
It is so hard to watch from the outside all of the blessed healthy families and not have some kind of sadness in my heart as that was just not our path. Our path is pain. We live in pain every single day. We know we are blessed to still have our children alive and for me to be able to continue to fight for all of us. However, I am tired. I am really, really tired of the fight. I want the fight to be over and to live a happy ever after…I want a Christmas Miracle – a diagnosis, treatment & cure.
When I went back to make our holiday card, I went through all of our pictures this past year. I see the happy pictures, which I used on our card. However, I had to go through the hundreds of medical pictures that I took along the way this year as well. As I look at my three beautiful children, I see their strength and their perseverance. When I look in the mirror. I see my failure. I see my failure as a mother for not being able to fix my children’s pain.
This trip is another round of hope. This trip is another round of trying to find answers. We can only pray for this new team to find something that all of the other incredible teams have not yet found. We have been working with the best of the very best for the past few years. We are even working with a new team here at the Children’s Hospital of Wisconsin. They are on the case too. They are incredible and working long hours to catch up on what they missed the past three years while we lived in Utah and since they saved Ava’s life during the summer of 2013. We are still working with the University Hospital in Salt Lake City, Utah, Intermountain Primary Children’s Hospital and the Utah Genome Project. We are working with MyGene2 and University of Washington Center for Mendelian Genomics (UW-CMG). We have an absolutely incredible group of brilliant doctors and researchers. It is time to find answers.
I want a Christmas Miracle – a diagnosis, treatment & cure.
To apply to the Undiagnosed Diseases Network (UDN)
About the Undiagnosed Diseases Network (UDN)
The Undiagnosed Diseases Network (UDN) is a research study that is funded by the National Institutes of Health Common Fund . Its purpose is to bring together clinical and research experts from across the United States to solve the most challenging medical mysteries using advanced technologies.
Through this study, we hope to both help individual patients and families and contribute to the understanding of how the human body works.
December 21st, 2016:
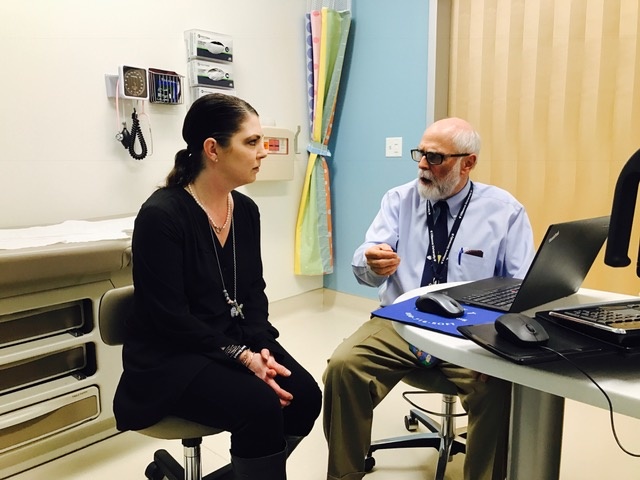
 Today is the one year mark for us with the Undiagnosed Diseases Network (UDN). Our applications landed on their desk last December, 21st, 2015. We are so very thankful to have been accepted into the UDN, a research study that is funded by the National Institutes of Health Common Fund , this year and to be working with their team in the UCLA Human Genetics at David Geffen School of Medicine at UCLA. We had hoped for a Christmas Miracle – a diagnosis, a treatment & a cure but our diagnostic odyssey will continue on in 2017. We feel very hopeful for the next steps in our journey. We were so impressed with the entire week, their program and their team. Dr. Stanley Nelson is our lead investigator with the UDN at UCLA Human Genetics. I loved meeting Dr. Nelson and learning more about his family and why he and his wife, Dr. Carrie Miceli, have dedicated their lives to helping the rare and undiagnosed disease community. Dr. Nelson is personally touched by rare disease. Learn more by reading: Two UCLA researchers combat lethal disease to save son and thousands like him: Their efforts have rallied others to the cause of defeating Duchenne muscular dystrophy as well as watching their video and reading their article in People Magazine: Two Scientists Vow to Find a Cure for Their Son’s Rare and Fatal Disease: ‘I’m Proud of the Work My Parents Are Doing,’ Says Teen
Today is the one year mark for us with the Undiagnosed Diseases Network (UDN). Our applications landed on their desk last December, 21st, 2015. We are so very thankful to have been accepted into the UDN, a research study that is funded by the National Institutes of Health Common Fund , this year and to be working with their team in the UCLA Human Genetics at David Geffen School of Medicine at UCLA. We had hoped for a Christmas Miracle – a diagnosis, a treatment & a cure but our diagnostic odyssey will continue on in 2017. We feel very hopeful for the next steps in our journey. We were so impressed with the entire week, their program and their team. Dr. Stanley Nelson is our lead investigator with the UDN at UCLA Human Genetics. I loved meeting Dr. Nelson and learning more about his family and why he and his wife, Dr. Carrie Miceli, have dedicated their lives to helping the rare and undiagnosed disease community. Dr. Nelson is personally touched by rare disease. Learn more by reading: Two UCLA researchers combat lethal disease to save son and thousands like him: Their efforts have rallied others to the cause of defeating Duchenne muscular dystrophy as well as watching their video and reading their article in People Magazine: Two Scientists Vow to Find a Cure for Their Son’s Rare and Fatal Disease: ‘I’m Proud of the Work My Parents Are Doing,’ Says Teen
This past Friday, we met with the team at noon. We recorded the conversation for Justin to listen to later. The discussion was very hopeful and the team is truly dedicated to finding a diagnosis for our family.
There is nothing in the data that we see right now that ties everything together. They will be reanalyzing my data as well as my parents’ data. Since nothing is obvious in the data as of now, they will go back to look for causes of my EOE, my arthritis and my dysautonomia. These are the three priorities for them at this time. They will look at the RNA sequencing from the muscle biopsy to see if there are any genes that are defective. They will look at different characteristics of the fibroblasts in the cells from the skin biopsy. This will all take at least another four months.
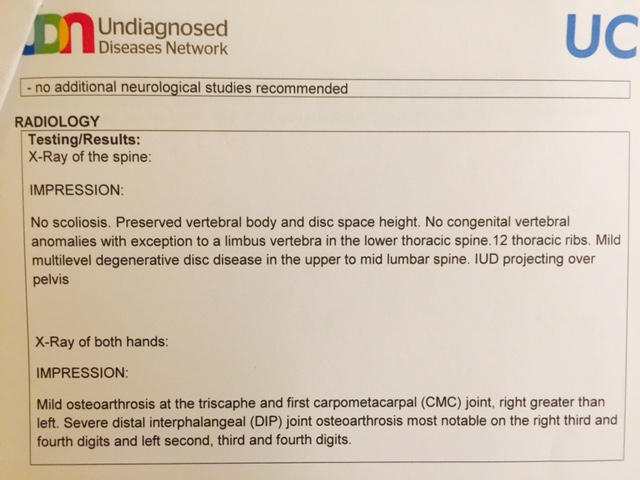
What was upsetting to me was that we learned from my hand X-rays is that not only are my distal interphalangeal (DIP) joints severe with osteoarthrosis, it is also now in my triscaphe and first carpometacarpal (CMC) joints. I wasn’t aware that it was in the next set of joints and I’m scared to death about the progression of my hands. I am only forty-three years old. What will they be like in twenty years? Both of my grandmothers also had crippling arthritis in their hands at an early age. I remember them in their later years and I remember what their hands looked like and how much pain they were in. If you think about everything you use your hands for and imagine crippling arthritis and pain, that is me. Typing, cutting food, laundry, cleaning, writing…it all hurts. I will now be searching for the top hand specialists in the country/world to find out what types of treatments are out there for slowing down the aggressive, progressive degenerative osteoarthrosis. If anyone has suggestions, I am listening!


 The UDN will continue to be working on our family. Matthew Herwog is my contact person at the UDN. We have been working together for a year now as of today!?! He wrote a wonderful email to me when we got back from our trip. I think he summarized it all very well:
The UDN will continue to be working on our family. Matthew Herwog is my contact person at the UDN. We have been working together for a year now as of today!?! He wrote a wonderful email to me when we got back from our trip. I think he summarized it all very well:
“Thank you for the kind words, and I know I can speak for everybody here that we likewise had a great time meeting all of you. I also know you were hoping for more concrete information (and ideally a diagnosis and treatments) from the visit, but I want to stress that even though it’s been nearly a year since you started your UDN journey with us (Your applications came to us on 12/21/2015), this is really just the beginning for us at the UDN. Now we get to utilize all of the resources available at UCLA and the UDN to start figuring out how the pieces fit together. It’ll still be a slow process (the latest bit of genetic testing we’re doing is cutting edge) and we might not find the answers right away, but we’ll keep plugging away until we have something.” – Matt
This is our eighth hospital in our fifth state. We are just so very thankful to have such amazing teams around the country focusing on our family. Thank you all from the bottom of our hearts.
We will continue to pray for a miracle in 2017 – a diagnosis, a treatment & cure.
Happy holidays and we pray for your family to be safe and healthy in 2017.
Thank you for your continued love, support and prayers.
Much love,
Gina
For more information about The Szajnuk’s UDN Visit
January 5, 2017: We are also going to be working with MyGene 2 and the University of Washington Center for Mendelian Genomics (UW-CMG). They will be analyzing our WGS as well. They sent us saliva collection kits to our home recently and we sent them back. It was incredible to be able to do it from our home and without drawing blood. We look forward to seeing their results as well.
February 11, 2017:
I was recently blessed with a trip back to Utah for the Utah Jazz game against our Milwaukee Bucks. I shared about my trip in my “RUN Family Changed My Life” blog. The week was very emotional but a huge success. I was able to meet with Dr. John Carey for a few hours along with my partner in crime, Jen Frisk. She sat in the meeting with us as she is undiagnosed and has three children that are undiagnosed. She spends hours researching her list of genes and her advice was invaluable to me.
We went over the WGS findings. He had two excel sheets to show me. He explained that the first excel sheet was a list of dominant genes found in me and found in the three children. The second excel sheet was a list of recessive genes found in me and found in the children. There were a lot of genes listed. We have a long way to go to find the smoking gun gene that is responsible for our disease process. We will continue on this journey in 2017. I am so very thankful to Dr. John Carey, Barry Moore and their entire team for dedicating so much time on our family. Thank you to the Utah Genome Project and Dr. Lynne Jorde and his team. We feel so blessed to have had our WGS done.
The children still suffer daily in pain and they miss a lot of school. Their only medicine is distraction. They are cognitively doing great but they have these bodies that do not work correctly. They persevere and are such an inspiration to me. They tell jokes and laugh often. They love their extended family and their friends. You only have one body in your lifetime. You have no choice except to fight for yourself and for your future. My three children have taught me to keep fighting for a diagnosis, a cure and a treatment. I want it for me as well. As a mother living with pain daily, I am scared for my future. I know what it feels like to feel just horrible. I lived my first thirty-four years as a healthy young woman. I was perfectly healthy. When I gave birth to Ava, my body changed. When I went through the stress of Ava’s four cranial surgeries and our move to Utah, my disease process progressed drastically. I just feel blessed to still have my Ava with me and that we have a very blessed opportunity to keep fighting for answers for all four of us and for all of the rare and undiagnosed community. This journey inspired me to do more. Much more.
April 27, 2017:
Update on our Undiagnosed Disease Network workup:
On April 24th, Dr. Howard Jacob coordinated a call between Dr. David Bick, Dr. Matthew Might, Dr. Stanley Nelson and with an outside company, GenePeek, to discuss our family. These are all major players within the Undiagnosed Disease Network and it was a huge honor to get them all on the phone together to discuss what their thoughts were and with what GenePeek had worked on for our family. Unfortunately, there still is no smoking gun gene to give us a diagnosis at this time.
Here is breakdown of what the UDN is doing for our family:
The first test was WGS, where we analyzed the sequencing of base pairs (ATGC) that make up your DNA. This was compared to reference genomes (genomes of individuals who don’t have known diseases or major medical symptoms) and also to the genomes of your family to help filter out the sequences that are known or expected to not cause any symptoms/disease. Initially, Dr. Nelson had out team look at variants in your DNA that were de novo (not inherited from your parents) and also shared in all 3 of your children. We did this under the thought that if all 4 of you shared similar symptoms, then the most obvious answer would be to look at the DNA that just the 4 of you shared. This came back with a handful of variants, but none of them were in clinical genes (genes known to cause symptoms/diseases) and none of them were in the coding regions of the genes (the most important part of the gene). Unfortunately for these types of variants it is very difficult to interpret how they might be causing any clinical symptoms. So now, Dr. Nelson wants to scale back, and just interpret your genome with regards to your parents, to see if he can’t find a better answer there, and then look at the genomes of your children to see if they share something similar.
We also ran RNA sequencing, where we look at the product of your DNA. Your DNA gets transcribed into RNA, which then goes on to do a variety of functions (regulate other parts of the genome, get translated into proteins/enzymes, and other very important cellular functions). RNA sequencing will tell us 2 important things:
First, is the gene being expressed (getting turned into RNA) more, less, or the same as we expect. If the expression of a gene is different from what we would expect, then we would expect there to be some consequence of the abnormal expression. We could then look at what the products of that specific gene, and it’s corresponding RNA, to see what that might be affecting. The major difficulty with analyzing RNA expression data is that it is highly dependent on the tissue type (ex. what’s expressed in your brain cells will be different than in your blood cells), and some genes just aren’t expressed in certain tissues.
The second thing RNA sequencing can tell us is how some of the non-coding DNA changes we find on WGS might be affecting the RNA that is produced by those genes. So we can look at the RNA sequence around the non-coding DNA changes to see if there are any abnormalities, and then also follow that up by looking at how that might be affecting the cell in a way that would be causing symptoms. The difficulty in looking at this part of the data is that in the vast majority of cases, the non-coding changes in the DNA aren’t affecting the RNA in any way that we can detect.
So the main benefit of running RNA sequencing is to pair it with the WGS to see if we can make more sense out of the DNA changes we don’t understand, and also to see if any of the genes are acting differently than we would expect for that tissue type.
The last genetic test that we ran on your family was looking at the structure of the DNA to see if there are any large abnormalities that would not be detected by WGS. So, if you imagine that your DNA is a book, then WGS will tell us all of the letters in the book, their sequence (how they are arranged), and it can detect if some of the words/letters are deleted or duplicated. What it can’t tell us is if any large parts of the book (pages, chapters, etc) are deleted, duplicated, or inverted (turned upside down), but the structural DNA test we ran can tell us that information. If we found a structural DNA change, then we would look at the genes in that region and see if they might explain the symptoms you are having.
April 27, 2017:
For a detailed update on the Szajnuk’s, please visit: Undiagnosed: An Update on the Szajnuks
May 9. 2017:
The Undiagnosed Disease Network posted my Participant Page 020. This was hard to read about myself but I am thankful to have other people around the world reading the page in hopes of finding more people like me. This has been a long journey and it continues on…
June 2nd, 2017:
June 16th, 2017:
It was such an honor to be a part of the Milwaukee Bucks this past year. It was a dream come true to be back in Wisconsin and near our family and friends.We want to thank everyone in the organization for their support of our family and of the Rare and Undiagnosed Network (RUN). We were so grateful for everything the Bucks did for RUN’s NBA Initiative this past year.
We are now looking forward to the next chapter in our lives.
September 13th, 2017:
November 17, 2017:

Ava Szajnuk’s CT on November 16, 2017: Technology is beautiful. Ava recently fell and hit her head in gym class. She suffered a head injury and a concussion. We are thankful it was not a skull fracture and that her shunt is working well. Ava wanted to share this picture with all of you. She is so proud of her shunt and to be able to see it in this incredible image was an amazing opportunity. We are so very thankful to technology. We have been blessed to have such a special team of doctors, nurses, teachers, family, friends and our rare and undiagnosed community. Ava continues to inspires me each and every single day to continue to move forward optimistically in our world of the unknown.
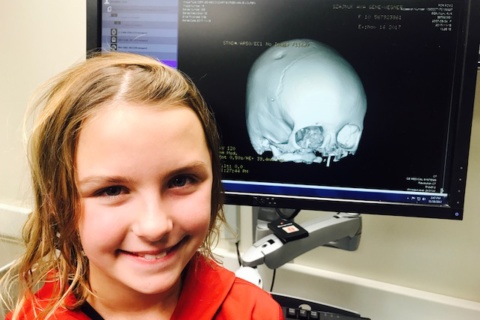
PS – Ava says, “Hi! Did you see my eyeballs?!”
We met with one of our neurologists back in Wisconsin last month. Dr. Kurt Hecox is an incredible doctor and a great investigator. We first met with him in May, 2016. He spent hours going through our records. He was enthusiastic and very kind. During our last visit, he was more somber. He had looked at all of the notes and even called other doctors around the country about our family. He came back to say that he unfortunately feels that we are twenty plus years ahead of science with our disease process. We do not have a smoking gun gene in our family and that we need to wait for the algorithm to search for multi gene disease processes. He suggested that we need to stop searching and to stop doing diagnostic testing until a new symptom appears. This was hard to hear. However, I already knew it deep down in my heart. After all of these years of traveling around the country and after all of the testing, we are in the same place we were when our first neurologist told me to just accept the unknown. She said that we will just need to treat the symptoms. I remember being so mad when she told me to just go buy a book about a mother raising a son for over twenty years that was undiagnosed. I was mad and I was not going to accept the unknown.
I’m never going to give up on trying to get a diagnosis, a treatment and a cure. However, we will take a break from our diagnostic odyssey and focus on our quality of life. We will wake up each and every day looking forward into our unknown future. We will be optimistic and we will not focus on our pain and our suffering. We will live each and every day to the fullest. We are doing well cognitively and we are fighting every single day. Thank you for being in our lives and for being such a huge support system. I do believe we gained an incredible network and community through our journey. We are forever grateful for the people we have met along the way.

We will continue to move forward one day at a time. However, I must admit that my heart hurts that we do not have an answer, a treatment and a cure by the end of 2017. Undiagnosed is still our diagnosis.

Well, if I went back to that very first neurologist, maybe I should ask her one very important question,
“What was the name of the book you wanted me to read?”

March 5th, 2018:
Global Gene’s RARE Daily: Learn more about RUN, our Mission and our Family
Written by Daniel Levine on the Global Gene’s RARE Daily on March 5, 2018
Rare Leader: Gina Szajnuk, Co-founder and Executive Director of Rare and Undiagnosed Network
March 17th, 2018:
RUN’s NBA Initiative: The Utah Jazz honored 30 rare and undiagnosed children and their families on the court as National Anthem Buddies on March 17th! Ricky Rubio and Alec Burks donated 100 tickets through the NBA Player Ticket Donation Program. The Milwaukee Bucks hosted our RUN families in a suite on March 2nd! Watch our KJZZ video from 2015 to learn more about our #RUNNBA!
April 13th, 2018:
“Before most rare disease patients have a name to give their condition, they go on a diagnostic odyssey than can take years and usually involves multiple specialists. For some patients, the answer never comes. In the absence of a diagnosis, patients face significant challenges getting the care they need, reimbursed by insurers, or necessary accommodations from schools or employers. Ahead of Undiagnosed Disease Day, which takes place April 29, we spoke to Gina Szajnuk, executive director of the Rare and Undiagnosed Network and Matt Might, Director of the Hugh Kaul Personalized Medicine Institute at the University of Alabama at Birmingham School of Medicine. They discussed what it’s like to be undiagnosed, efforts to raise awareness about the plight of undiagnosed patients, and why “undiagnosed” is a diagnosis.”
Global Genes RARE Cast: When “Undiagnosed” Is Your Diagnosis
by Daniel Levine and Levine Media Group
April 27th, 2018:
Ava spoke to the University of Utah School of Medicine’s medical students.
“Hi. My name is Ava Szajnuk. I am ten years old and I have an undiagnosed rare disease. Some people ask, “Why do you hurt?” and I say, “If we knew that, I would already be cured.” Imagine it, like every normal person was a brilliant blue sky, and I, am a raging hurricane Harvey!”
August 16th, 2018:
Gina Update: Since my visit to the UDN in 2016, the University of Utah has now added Fibromuscular Dysplasia (FMD) and Median Arcuate Ligament Syndrome (MALS) to my list. I am in the process of learning more about these two new diagnoses and exploring my options. I still feel at the starting line and am working daily to see what is out there in both Western medicine as well as Eastern medicine.
September 12th, 2018:
I just checked into my MyGene2.org and found out I have 32 candidate genes listed for our family!
Family ID: 96
Number of candidate genes: 32
The following gene(s) are “candidate genes” for this family’s genetic condition, which means any one of these genes and the variants in them (i.e., candidate variants) could be responsible for the condition. There may be one or many candidate genes in each family. The presence of more than one candidate gene reflects uncertainty about which specific gene is responsible. It is also possible that the underlying gene is not listed as one of the candidates.
NAGA, DBH, SPG11, SPR, ATXN, TSFM, AGRN, ITPKC, FOXE1, TNXB, GALT, SLC12A6, ATXN1, ANK2, F10, MICAL2, CNOT1, DALRD2, MEGF9, ANP32B, MSRA, NCOA1, ATRAID, PAPOLG, MCF2L2, SHKBP1, MUC16, SIRPG, AGT, FAM186A, DACH1, PIK3C2A
January 20th, 2019:
I turned forty-six years old today. I am still undiagnosed and my children are still undiagnosed. We persevere every single day. Ava and I both cried this week…”Why can’t I feel better?”
I spent my forty-fifth year doing another deep dive into my health in the hopes of finally figuring out the root cause. No deal.
However, I did receive five more diagnoses to add to the list. Connective Tissue Disease, Cervicogenic Headache, Fibromuscular Dysplasia (FMD), Hypertension and Median Arcuate Ligament Syndrome (MALS).
For all of my diagnoses: Gina Szajnuk’s UDN Participant Page
The level of pain from my cervicogenic headache is absolutely a ten out of ten. I have had this since March, 2018. Seven procedures have been done and still no relief. I continue to advocate for our family in the hopes of eventually finding a diagnosis, a treatment and a cure.
My dream has always been collaboration, collaboration, collaboration. Through our journey we have had our whole exome sequenced and analyzed over six times now. We have had our whole genome sequenced and analyzed over three times. I am blown away by the number of people truly invested in helping our family find a diagnosis. Without sharing our journey, we would have been so alone in this diagnostic odyssey. Sharing our data with different eyes and with the top people in the field of genetics has always been my dream not only for our family but for all of the families living in a diagnostic odyssey. We are breaking down the silos! We are getting people to work together and outside of their four walls. It is an exciting time in genetics! We have so many people dedicating their time and energy to helping our family. We are forever grateful to each and every single one of you.
My dream also continues to have whole genome sequencing for everyone in the beginning of the diagnostic odyssey instead of years into it and to have it covered by their insurance company. It’s a huge dream but it is the future. Let’s all pray it happens sooner than later. The more people sequenced, the more genes we will find. When we all start sharing the data, we will be able to connect the dots more and hopefully start diagnosing the Undiagnosed. One can only dream. One can keep fighting for answers. I will dream. I will keep fighting. I want a diagnosis, a treatment and a cure.

RUN’s Two Year Anniversary Video by Small Forces
RUN’s One Year Anniversary Video
#UndiagnosedDay RUN’s 2016 Video
About
Gina Szajnuk (Zanik) was born and raised in Madison, Wisconsin. She serves as the Co-founder and Executive Director for the Rare and Undiagnosed Network (RUN), a 501©3 nonprofit organization formed in 2014. Her three children, each of whom live with an undiagnosed rare disease, continue to inspire and motivate her to empower rare and undiagnosed patients and their families with genomic information and community through advocacy, networking and support. Gina is also living with an undiagnosed rare disease. In 2016, Gina was the Chair of Utah Rare and made Utah the #1 state for Rare Disease Day. She was on the Executive Committee for Utah Rare for four years. Gina continuously works to build a network of rare advocates, geneticists, researchers, specialists, and volunteers who can come together under one platform. In 2016, RUN started the Undiagnosed Rare Disease Day awareness campaign on April 29th. The campaign became an international awareness day and has been celebrated yearly. She is Vice Chair of the Utah Rare Disease Advisory Council (RDAC). She is a Board Member of the Metrodora Institute’s Foundation. She serves as a Patient Advocacy Advisor on RARE-X as well as a Patient Advocacy Advisor for the Undiagnosed Disease Network Foundation (UDNF). She was a member of the Participant Engagement and Empowerment Resource (PEER) of the Undiagnosed Diseases Network (UDN) for two years. RUN is a member of the Undiagnosed Disease Network International (UDNI) as well as the Rare Disease Diagnosis Consortium. She was a member of The Rare Advocacy Movement (RAM) for two years. She served as the National Organization for Rare Disorders (NORD) as their Utah State Ambassador and then as their Undiagnosed Advocacy Ambassador for four years. She is a public speaker and a contributor to the MediaPlanet’s Rare Diseases Campaigns as well as The Mighty. She is married to Justin Zanik, the NBA Utah Jazz General Manager. Through her husband’s position in the NBA, Gina has brought awareness to the NBA about the importance of rare and undiagnosed diseases through RUN’s NBA Initiative started in 2015. In 2016, Gina won the Rare Voice Award from the EveryLife Foundation for Rare Diseases as well as accepted the Rare Champion of Hope – Advocacy Award from Global Genes. She graduated with a Bachelor of Arts from the University of Wisconsin – Madison.